What is celiac disease?
Celiac disease is a condition in which a person develops inflammation, or swelling, and damage to their intestine (gut) when they eat gluten. Some of the symptoms of celiac disease are gas, stomach bloating and pain that does not go away, diarrhea and constipation. Fatigue and headaches are also common.
The gluten-free diet (GFD) is the only treatment for celiac disease. In many patients with celiac disease, even a small amount of gluten is enough to cause harm, even though they may not feel symptoms. A lifelong GFD will help protect the small intestine and may be able to undo damage that has already happened.
What happens in your gut if you have celiac disease
-
Small intestine
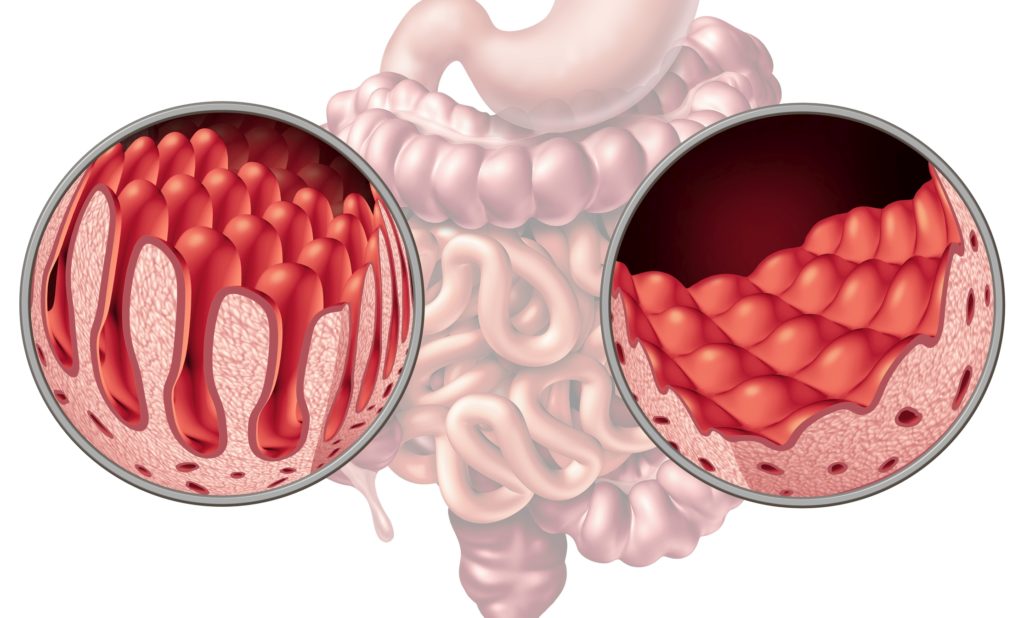
The small intestine, which is about 20 feet long, finishes the process of digestion, takes in the nutrients, and passes the leftover material on to the large intestine for elimination. The small intestine is lined by tiny, fingerlike protrusions, called villi.
-
Villi
Villi absorb nutrients from food. Celiac disease hurts the villi.
-
Malnutrition
Without healthy villi, nutrients will pass through the small intestine without being absorbed and you may become malnourished and deficient (lacking) in some vitamins and minerals.
What are symptoms of celiac disease?
Common symptoms
* Gas, belly bloating and pain that doesn’t go away.
* Diarrhea (loose stool) or constipation (hard stool or trouble passing stool) that doesn’t go away.
* Pale, foul-smelling or fatty stool.
* Weight loss.
* Tiredness or low energy levels.
* Changes in behavior; irritability in children.
* Tingling or numbness in the legs (from nerve damage).
* Bone or joint pain.
* Muscle cramps.
* Delayed growth in children.
* Pale sores inside the mouth.
* Itchy skin rash.
* Brain fog.
Having these symptoms does not mean you have celiac disease. If you think you may have celiac disease, do not get rid of gluten from your diet until your doctor has tested you. It is important to talk with your doctor about options and discover the cause of your symptoms
Some patients with celiac disease do not have symptoms. Other clues that a person has celiac disease include:
- Having a close family member with celiac disease (parents, siblings, children).
- Anemia or low red blood counts.
- Elevated liver numbers (AST, ALT, alkaline phosphatase).
- Osteoporosis (weakened bones).
Who gets celiac disease?
Celiac disease is not a rare disease. Recent research has shown that as many as 3 million people in the U.S. (about 1% of the population) may have celiac disease.
Celiac disease can be found in both children and adults and people may live for years without knowing they have it. In some patients, the disease shows itself after an event such as surgery, pregnancy, viral infections or severe emotional stress.
Demographics
While most people in the U.S. who have celiac disease are non-Hispanic White, people who are Black and Hispanic can have celiac disease.
All people with celiac disease have at least one copy of a celiac gene (HLA-DQ2 or HLA-DQ8). People with Northern European ancestry commonly have one of these genes. So, doctors thought that mainly people of Northern European ancestry developed celiac disease. However, we now know that people from many different parts of the world have celiac disease, including the U.S., Mexico, Latin America, India, and China.
To our best knowledge, most people with celiac disease (70% or more) in the U.S. are non-Hispanic White. Little is known about celiac disease in Blacks and Hispanics in the U.S., including what proportion have celiac disease, if they are tested for celiac disease at the same rates, if they have different symptoms, or if their lab tests are different than non-Hispanic Whites.
Autoimmune disease and celiac
What are the tests for celiac disease?
After talking about your symptoms with your doctor, tests for celiac disease may be performed. As celiac disease is a lifelong health issue, a correct diagnosis is very important.
If you think you may have celiac disease, do not get rid of gluten from your diet until your doctor has tested you.
Blood test
A blood test is the most common test, as it is easy and can give a clear answer. Results often take about a week.
A blood test to see if you have celiac disease can only work if you are eating gluten, so be sure to keep gluten in your diet before testing is done. (Only limit gluten from your diet if your doctor tells you to do so.)
Based on the results, your gastroenterologist may wish to do an endoscopy.
Endoscopy
An endoscopy is done to get small pieces of tissue (biopsies) from your small intestine to see if there is damage stopping your body from taking in nutrients, caused by celiac disease.
You will be given medicine to block pain and make you feel relaxed and sleepy, so you won’t feel much during the test. During the endoscopy, your gastroenterologist will use a long, thin (about the width of your little finger), flexible tube with a camera on the end to look inside. The tube is passed through the mouth into the small intestine as your gastroenterologist does a careful exam to check for damage.
Getting a biopsy before starting a gluten-free diet gives you and your doctor proper baseline data to be used if issues come up in the future, so be sure to keep gluten in your diet before testing is done. (Only go gluten-free if your doctor tells you to do so.)
Endoscopy is the best way to show that you have celiac disease and the best way to make sure your intestine heals the right way.
Other tests
Your doctor may do a genetic test to see if celiac disease can affect you if there is uncertainty as to the diagnosis, such as when you have been gluten free before testing. Note the genetic test does not prove the diagnosis but helps direct further diagnostic efforts.
While other types of tests, such as saliva and stool tests, may be offered, these are not accurate and should not replace the blood test and endoscopy.
If your tests do not show celiac disease, some choices your doctor may give you are:
- Taking a gluten challenge to look for gluten intolerance. Your doctor can give you more information on how to do this and if it would be helpful.
- Tracking your diet, which can help find other possible food allergies and intolerances, such as to lactose or fructose.
Newly diagnosed with celiac disease
No matter what you may be feeling upon hearing you have celiac disease, you are not alone. Many places have support groups for people with celiac disease, both in-person and online, that can be very helpful. If you are overwhelmed by your new diagnosis, don’t wait to reach out to a mental health expert to talk through the changes. Relaxation techniques, such as yoga, meditation or mindfulness may be very helpful.
Start a gluten-free diet (GFD)
Good news! You should start feeling better within weeks of changing your diet. Your gastroenterologist will give you information on the GFD to heal your intestine and (hopefully) get rid of your symptoms.
Starting a gluten-free diet has a big learning curve and accidents are common early on. This is normal but being exposed to even small amounts of gluten may make your symptoms worse. This is often not planned and may come from unexpected sources of gluten, such as cookware (if it has been used to cook food that has gluten), salad bars and certain medications. Your doctor or dietitian can help you find and learn about these hidden sources of gluten.
While you may be tempted to cheat and may not notice much of a problem when you do, it is important to keep in mind that your intestine will still be harmed by gluten, it will not heal, and you may run the risk of long-term problem. Know that some patients may gain weight with celiac disease and also on the GFD. Some patients may have constipation, which means they have hard stool or trouble passing stool.
Symptoms that do not get better on the GFD or return after going away can have many causes. Thankfully, most of these are simply treated, but rarely this may be due to refractory celiac disease, which would need treatment with medications along with the GFD.
Additional testing
Your doctor will also talk with you about testing for vitamin and mineral deficiencies or other problems linked to celiac disease. Many celiac disease patients do not have gastrointestinal (GI) symptoms, but may have thyroid disease, anemia (too little iron in the blood), osteoporosis (weakened bones), liver disease, or females may have gynecologic issues (irregular periods and infertility).
Plan to see your doctor regularly. Your doctor may do check-up tests (like blood tests or an endoscopy) to see your progress.
Patients may go through depression (low mood) or anxiety (worry), or have trouble coping with celiac disease. These are all normal responses to finding out you have celiac disease. If you are having any of these feelings, reach out to a mental-health expert right away.
You should also receive an annual flu vaccine and pneumococcal vaccine.
Consult a registered dietitian
Know the complications of untreated celiac disease
* People with untreated celiac disease are at a greater risk of not getting enough nutrients, like vitamin D and iron.
* Patients with untreated celiac disease may have weak or brittle bones; children may be short for their age.
* Patients not being treated may have a slightly greater risk of lymphoma and intestinal cancers.
* Some patients with celiac disease may have other autoimmune problems, such as Type 1 diabetes, thyroid disease and liver disease, among others.
Diet and support
The gluten-free diet (GFD)
- Wheat.
- Barley.
- Rye.
- Malt.
- Brewer’s yeast.
- Oats (unless they are pure, uncontaminated, labeled gluten-free oats and your doctor has said you are able to eat them).
- Yeast extract and autolyzed yeast extract (avoid unless a non-gluten source is indicated on the label).
- Lip balm, lip stick, and lip gloss.
- Any make up that could come in to contact with your lips.
- Shampoos.
- Hand sanitizer (if not gluten free, wash hands before eating).
- Hand lotion (if not gluten free, wash hands before eating).
- Playdough (if not gluten free, wash your hands after using).
- Medications and supplements can contain gluten as an additive. Call the manufacturer and check DailyMed.
Just like a diet without any limits, eating a balance of each food group will help to keep you healthy.
- Fruits and veggies (fresh, frozen or canned without sauces or flavors); plain meat, fish, and poultry; plain nuts and seeds; oils; and most milk products are all naturally gluten-free.
- No need to skip the starch. There are plenty of gluten-free grains and starches you can eat. Remember, whole grains are part of a balanced diet, too. These can be consumed on a GFD: rice, potatoes, sweet potatoes, corn.
- Try some of these higher fiber, nutritious gluten-free grains and starches that act like grains: amaranth, quinoa, millet, sorghum, buckwheat, teff. (Make sure they are labeled gluten-free!)
- There are many gluten-free replacements for common snacks and foods like crackers, cereal, pasta, baking mixes and more. If it is labeled “gluten-free,” it is safe to eat. If a product is not labeled gluten-free but has no gluten containing ingredients, call the manufacturer as manufacturers are not required to use the gluten-free label.
Having to follow a gluten free diet during holidays, special occasions, and family or religious traditions can be hard. Don’t let celiac disease prevent you from celebrating or socializing! Talk to your friends and family about your dietary restrictions ahead of get togethers. Coming up with a strategy to eat gluten free and feel included is important.
Have a recipe for a special dish? Take the recipe with you to the dietitian. They may have tips for substitutions or adaptations to make the recipe gluten free. Look for a similar recipe online or in a gluten free cookbook.
Don’t feel bad about using a mix instead of baking from scratch. Let someone else find the right combination of flours so that you can enjoy the rest of the process.
Plan ahead! Sometimes gluten free cooking and baking takes trial and error to get the desired result. Ask friends or look online to see which flour blends are best used for different baked goods. Sometimes, the substitutions and similar recipes just are not quite the same. Consider a new gluten-free tradition that reminds you of the original.
Check out local restaurants and bakeries for pre-made individual or family-style gluten free holiday meals.
Catholicism, Christian – Holy communion or eucharist
- Receive wine or juice only.
- Take care to use a separate paten, pyx or communion plate for gluten free bread or wafers to avoid cross contamination.
- Take care to use a separate chalice for drinking or intinction to avoid cross contamination.
Judaism – eating matzah on Passover or challah on Shabbat
- Use gluten-free oat matzah instead. Check with your doctor that you are able to eat oats first. If you are unable to eat oats, check with your rabbi to be excused temporarily.
- Bake or buy gluten-free challah.
Celiac disease should not stop you from eating out. There are more new gluten-free choices each day, so start exploring! Here are a few tips to keep in mind when eating out:
Know the gluten-free diet!
- Be sure you have solid knowledge of labels and what you can safely eat.
- Don’t forget about hidden gluten in salad dressings, soups, marinades and fried foods.
Let your server (or host) know.
- Speak up! Make sure they know you cannot have items with gluten or that have been in contact with gluten, including gloves, cutting boards, utensils and pots.
- Ask questions. Sometimes it helps to call and ask questions before arriving.
- Not sure how a menu item is made? Ask your server to ask the kitchen staff. Better safe than sorry.
- Don’t see a gluten-free menu right away? Try asking! They may have one that you need to request.
- Send it back (if you need to). Mistakes happen and that is OK. However, if the staff makes a mistake and adds gluten to your dish (such as putting croutons in your salad), you need to ask for it to be fixed.
- Say thank you. Needing to change something is nothing to feel guilty about. Showing your thanks and kindness goes a long way.
- Do your research. With so many restaurants having gluten-free menus, try a quick Internet search to find new places.
What successful treatment looks like
Being healed from celiac disease means that your small intestine starts to work as it should again and can start taking in nutrients the right way. Your celiac blood tests and vitamin levels return to normal, but this does not mean that you are able to eat gluten.
While you will never be fully cured of celiac disease, meaning you will always have the disease, after eating a GFD, your small intestine usually heals within two years for adults and within a few months in children and young adults. Your gastroenterologist may want to take another biopsy (taking a small piece of tissue to look at under a microscope) about one to two years after you start to make sure your new diet is helping.
The National Institutes of Health suggests these points to keep in mind as you care for your celiac disease
-

Consultation with a skilled registered dietitian (RD)
* Ask your GI doctor for a recommendation.
* Use the AGA Find a Health Care Provider tool.
* Perform a Google search for registered dietitians in your area who specialize in celiac disease. -

Education about celiac disease
* Get and stay informed. Trusted websites, like government sites, can give you great information.
-

Lifelong adherence to a GFD
* Even a little bit of gluten can go a long way in terms of harming your gut. Learn the best ways to eat gluten-free while still keeping up your daily routines.
-

Identification and treatment of nutritional deficiencies
* This means having routine health exams so you doctor can check blood levels of certain vitamins, minerals and nutrients.
-

Access to a support group
* There are plenty of community groups that focus on celiac disease. Reach out and get connected.
-

Continuous long-term follow-up by a multidisciplinary team
* Since celiac disease stays with you your whole life, you need to create a good, long-term relationship with you doctor and dietitian. Be open with them about symptoms, questions or concerns.
Still having symptoms?
It can be scary to keep having symptoms, even after changing to a GFD. There are a few courses of action to think over when this is the case:
- Are you still eating gluten while on the gluten-free diet? Remember, even a little bit of gluten can have a harmful impact.
- Are you possibly consuming hidden gluten? A dietitian can help you find out if you are unintentionally consuming gluten through such things as medications, supplements or other sources.
If the answer is no to these questions and you have been on a GFD for at least six months, it is time to meet again with your gastroenterologist to find out if more tests or treatment options are needed. Try a symptom tracker or simple pen and paper to note your symptoms and when they occur.
Support groups
Reviewed by

Amanda K. Cartee
MD
Clinical lecturer, University of Michigan, Ann Arbor, Michigan