What is IBD?
Inflammatory bowel disease, or IBD, is when there is inflammation, or swelling, in the gastrointestinal (GI) tract and a lifelong immune response. The disease causes the body and immune system to think that food, bacteria and other needed things in the intestine are not supposed to be there. With this, the body attacks the cells of the bowels, causing inflammation that does not easily go away. Nearly 3 million Americans are affected by IBD, and the number of people affected continues to grow worldwide.
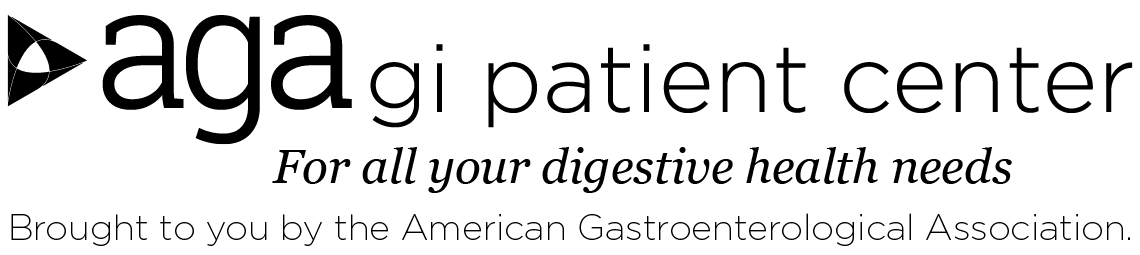
There are two main types of IBD: ulcerative colitis and Crohn’s disease. Both are illnesses with times of remission (when you feel well) and relapse (when you feel ill). Symptoms can differ from person to person and depend on the type of IBD.
Who does IBD affect?
- IBD affects both men and women.
- IBD is often found in people in their late teens and 20s, though it can be found at any age.
- IBD is found in people of all races and ethnicities across the globe. It is increasing in minorities and immigrants to industrialized countries, as well as in countries in Latin America, Asia and Africa.
Coping with IBD
Though IBD is a long-term health issue that has times of remission and relapse, most people have a normal life span and a good quality of life. For those who have chronic and continuing symptoms, here are a few tips to try:
- Know your body and how IBD affects you.
- Learn to care for yourself — have control over those things you can control.
- Build a support system that works for you: family, friends and support groups.
- Be sure to follow instructions from your medical team.
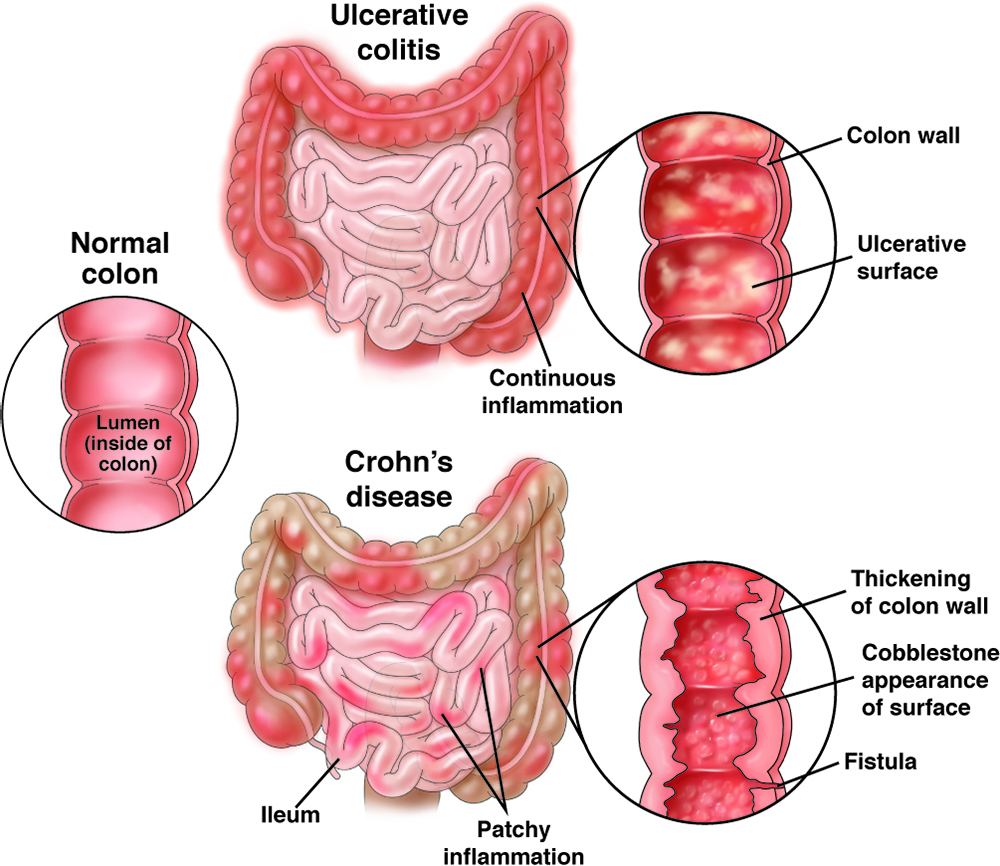
Ulcerative colitis
Ulcerative colitis (UC), which is more common than Crohn’s disease, is an inflammatory disease involving the large intestine (rectum and colon). It may affect part or all of the large intestine. Individuals with UC will often have:
- Bloody, loose stool.
- Urgency, or immediate need, to go to the bathroom.
- Increased number of bowel movements.
- Abdominal pain and cramping.
Some people with UC may have weight loss or other systemic symptoms (symptoms that affect the entire body). The inflammation of UC can also affect the joints or skin, leading to painful joints and skin rashes. During a flare-up, symptoms may go beyond those that affect the digestive system, including:
- Rashes or patches of red, swollen skin.
- Painful or swollen joints.
- Mouth ulcers.
- Red, irritated eyes.
Skin problems affect up to 15% of people with IBD. The disease may start slowly and progress for several weeks.
UC can be characterized as being in remission (time when the symptoms get better) or mildly, moderately or severely active. It can also be described as fulminant, which means that it is severely active and not responding to therapy.
Key terms
No blood or urgency and normal bowel function.
Fewer than four stools per day (with or without blood) without other symptoms and normal inflammatory markers.
Four or more bloody stools per day with minimal signs of other symptoms in the body.
More than six bloody stools per day with signs of systemic effects such as:
- Fevers.
- Abnormally rapid heart rate.
- Anemia (red blood cell deficiency).
More than 10 bloody bowel movements per day. May also have other symptoms, including abdominal swelling or the need for blood transfusions.
UC is diagnosed by the presence of the common symptoms and endoscopic and biopsy (small tissue sample) findings of chronic inflammation in the large intestine. Read more about ulcerative colitis.
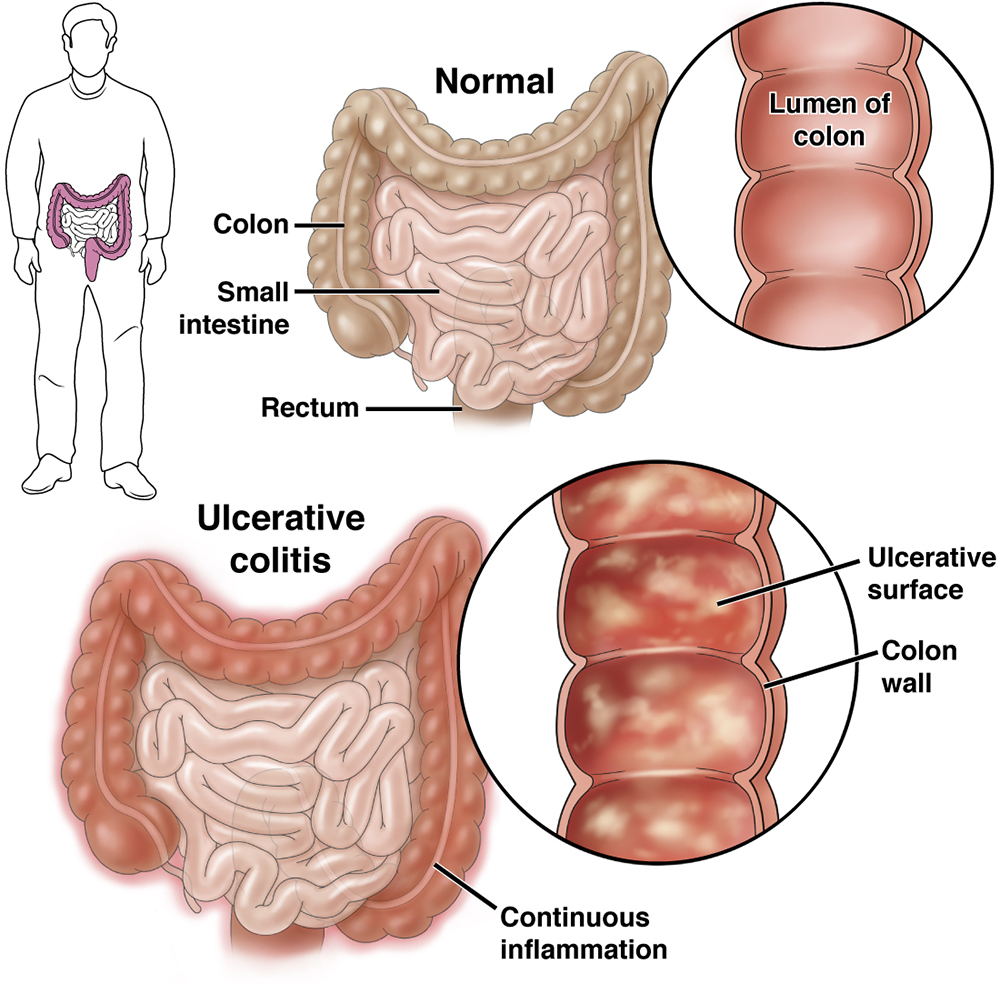
Crohn’s disease
Crohn’s disease may affect any part of the digestive tract, with the ileum (the final part of the small intestine) being the most common site for the disease.
Crohn’s disease is often characterized by abdominal (stomach) pain, diarrhea and weight loss, and sometimes with an abdominal mass, intestinal blockage or fistula. About 20-25% of patients with Crohn’s disease may have a fistula. A fistula is an abnormal connection between the intestinal tract and another structure that usually occurs in the anal area, but the fistula may also occur if the intestine is normal. Perianal disease (fistulas, fissures or ulcers near the anus) has been reported to be more frequent in Black, South Asian and Hispanic people.
The exact causes of Crohn’s disease are unknown, although several genetic and environmental factors may increase the risk of the disease. Read more about Crohn’s disease.
IBD disease management strategies
Because IBD may be a progressive disease (meaning it can get worse over time), early diagnosis and treatment have the potential to impact disease. The time from the onset of the symptoms, or when a person starts to feel unwell, to when the diagnosis is made is important.
The diagnosis of IBD usually requires evaluation by a gastroenterologist. Depending on your health coverage, you may need a referral from your primary physician or authorization from your medical insurer for this evaluation.
The therapeutic window of opportunity — meaning treating earlier in the disease — is also important to make sure the disease doesn’t quickly worsen with more serious problems. This is important because, many times, a diagnosis may be delayed because other conditions, such as irritable bowel syndrome, lactose intolerance or hemorrhoids, are mistakenly considered instead. Limitations in the access to subspecialty care may also result in a delay in diagnosis and treatment.
The other reason the diseases may progress is if treatments are not used as directed or are used improperly and deeper levels of control and remission are not achieved. According to recent research, the average times from the beginning of symptoms to the diagnosis of disease were 8.3 and 4.5 months for Crohn’s disease and UC, respectively.
Management of IBD differs for each patient and depends on the exact location of the disease, the type of symptoms and the severity of the disease. The general goals for managing IBD are:
- Get rid of the symptoms of disease.
- Improve quality of life.
- Promote and enable normal, unrestricted activity.
- Avoid hospitalizations, emergency department visits and disability.
- Avoid steroids.
Gastroenterologists focus on both helping their patients into remission, which is the absence of symptoms, and then maintaining remission or preventing flare-ups.
From a medical view, the goal of treating IBD is mucosal healing/deep remission, which means the patient feels well and does not show signs of inflammation. Mucosal healing, which is described as not seeing disease activity or ulcers during colonoscopy or other imaging tests, is also becoming more important in the management of IBD.
When mucosal healing is achieved in both Crohn’s disease and UC, a patient is less likely to have flare-ups, hospitalizations or surgeries. When remission is achieved, the health care team may tailor treatments to maintain remission.
Other goals of long-term treatment include reducing the use of steroids for a long period of time and reducing the long-term risk of colorectal cancer (CRC). People who have UC or Crohn’s disease involving the large intestine have a higher risk of developing CRC compared with those who do not have these conditions, but this can be prevented with the correct treatment of the disease and routine colonoscopies. The risk of cancer is decreasing with better treatments and prevention strategies. Given that some treatments for IBD can have rare but potentially serious side effects, gastroenterologists work with patients to weigh the benefits and risks of the different medicines with the risk of untreated, or undertreated, disease.
Patient risk stratification means finding patients who are at higher and lower risk for complications. Early identification of these high-risk features could help prevent long-term problems. Patients with complicated disease, or high-risk features, include:
- Patients with fistulas (connections between the intestinal tract and another place).
- Patients who need surgery for their IBD.
- Patients who have a lot of inflammation (i.e., a lot of the intestine is involved).
- Patients who are young when first diagnosed.
- Patients who smoke cigarettes.
- Patients who have many flare-ups and need to use steroids.
If a patient has one of more of these high-risk features, it is very important that the disease is managed by an experienced gastroenterologist with expertise that includes IBD.
Getting tested for IBD
Your health care team may order blood tests or stool studies to help with the diagnosis and to evaluate, or measure, your response to medication or make sure there are no side effects to the medication.
Your gastroenterologist will often order an imaging or radiology test, such as computed tomography (CT scan) or magnetic resonance imaging (MRI) to measure the degree of inflammation or if there is concern about an abscess or other complication from IBD.
IBD treatment strategies
Treatment for IBD may include medical management, surgical interventions, complementary/ alternative medicine (CAM) or lifestyle changes (such as quitting smoking).
It is important to talk about any treatments or changes to treatment with the gastroenterologist.
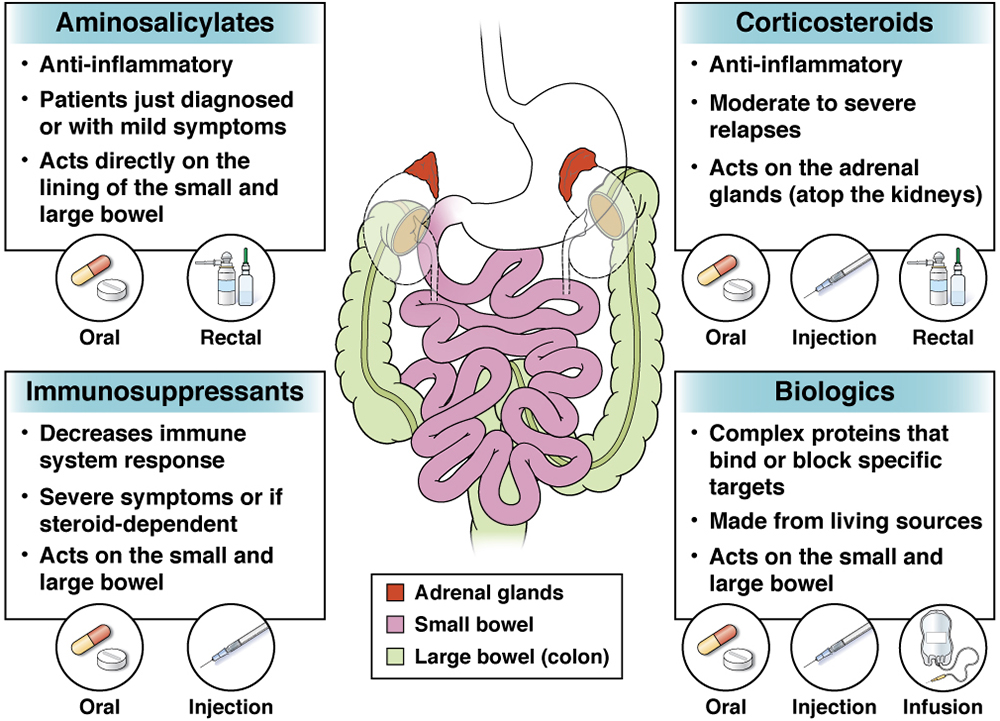
Several types of medicines are often used to manage IBD, including aminosalicylates, steroids, immunosuppressants and biologics.
Medical management
Anti-inflammatory medications used to help control or reduce inflammation in the digestive tract. They work directly on the lining of the bowel, especially in those who have just been diagnosed or those with mild symptoms.
Mesalamine, also known as 5-aminosalicylic acid (5-ASA), is the active component believed to deliver the anti-inflammatory effects via oral (by mouth) or rectal (by rectum) delivery. Examples include:
- Sulfasalazine (brand name: Azulfidine®)
- Mesalamine (brand names: Asacol®, Pentasa®, Apriso®, Lialda®, Delzicol®)
- Balsalazide (brand names: Giazo®, Colazal®)
- Olsalazine (brand name: Dipentum®)
Sulfasalazine, balsalazide and olsalazine are oral medications that work in different ways to lessen inflammation in the large intestine (colon and rectum).
Mesalamine is available in many oral and rectal forms, each of which targets different parts of the digestive tract. The most common side effects with 5-ASAs include headache, diarrhea, bloating and nausea. Patients taking 5-ASAs should be seen regularly by a health care team to check for side effects.
Also known as steroids, strong anti-inflammatory agents used to treat moderate to severe relapses of IBD. They act by slowing down multiple inflammatory pathways.
Corticosteroids are available in oral, rectal and intravenous (medicine given directly into a vein) forms. When people take corticosteroids, their adrenal glands slow down or stop making cortisol, a hormone naturally made by the body’s adrenal glands.
For people with moderate to severe active IBD, corticosteroids include:
- Prednisone (brand name: Deltasone®)
- Methylprednisolone (brand name: Medrol®)
- Hydrocortisone (brand name: Cortef®, Cortril®, Hydrocortone®)
- Budesonide (brand names: Entocort® EC, Uceris™)
Budesonide is part of a new class of corticosteroids called nonsystemic steroids because they target the intestine rather than the whole body. By doing so, they cause fewer side effects. Budesonide capsules are designed to slow the release of budesonide until the drug reaches the ileum and ascending colon.
The side effects of corticosteroids are affected by the dose and length of treatment. They are only recommended for short-term use to reach remission, because they are not effective at preventing flare-ups. Long-term or frequent use of these steroids is not recommended because of their undesirable side effects.
New formulations of glucocorticosteroids have been introduced with the goal of the same effectiveness of steroids already available but with fewer side effects. Some common side effects of corticosteroids include:
- Increased appetite and weight gain.
- Face puffiness.
- Increased facial hair.
- Night sweats.
- Trouble sleeping.
- Mood changes.
- Hyperactivity.
Some longer-term (i.e., when steroids are taken for more than six to 12 months) side effects include diabetes mellitus (poor control of sugar) and osteoporosis (thinning of the bones).
Medicines that decrease the normal immune system response. These drugs are used to control severe symptoms or when a patient cannot stop taking steroids. They are also used in combination with biologics (see below). They are safe, but liver function and white blood cell counts need to be regularly checked.
Oral medicines
- Azathioprine (brand name: Azasan®, Imuran®)
- 6-Mercaptopurine (6-MP; brand name: Purinethol®, Purixan®)
- Tofacitinib (brand name: Xeljanz®)
- This is an oral medication approved for moderate to severe UC that works by inhibiting the Janus kinase (JAK) protein family, which consists of JAK 1, 2 and 3 and the related kinase tyrosine kinase 2.
Injection/shot
- Methotrexate (brand name: Abitrexate®, Folex®, Mexate®) Note: this drug can cause miscarriage and must not be taken during pregnancy because it can cause deformities in the fetus.
Possible side effects include:
- Nausea or vomiting.
- Diarrhea (loose stool).
- Decreased ability to fight infections (because of a low white blood cell count).
- Fatigue or feeling tired.
- Pancreatitis.
Complex proteins designed to bind or block specific targets. Biologics are made partly or completely from living biologic sources, such as animals and humans. They have active ingredients, such as antibodies or hormones, and include a broad range of drugs, differing in how they work and how they are given.
A biosimilar is a biologic based on an existing (originator) biologic but is not an exact copy. Biosimilars work the same way as their originator biologics and are given the same way.
Many types of biologics are available to treat IBD. These biologics are given either orally, by injection (a shot under the skin) or infusion into a vein.
Tumor necrosis factor (TNF) antagonists bind and block a small protein called TNF-α, which is linked to swelling in the intestine and other organs and tissues. TNF antagonists lessen the symptoms of IBD and help healing of an inflamed intestine. Examples include:
- Adalimumab (brand name: Humira®)
- Certolizumab brand name: (Cimzia®)
- Infliximab (brand name: Remicade®)
- Infliximab-abda (brand name: Renflexis), Remicade biosimilar
- Infliximab-dyyb (brand name: Inflectra), Remicade biosimilar
- Infliximab—axxq (brand name: Avsola), Remicade biosimilar
- Golimumab (brand name: Simponi®)
Integrin receptor antagonists block a protein on the surface of cells and prevents them from moving out of the blood vessels and into tissues. An example is: Vedolizumab (brand name: Entyvio®)
Interleukin (IL) 12 and IL-23 antagonists block two cytokines (chemicals made by cells that affect other cells, specifically IL-12 and IL-23) from causing swelling in Crohn’s disease and ulcerative colitis. An example is: Ustekinumab (brand name: Stelara®)
Every medication balances how well it works with potential side effects. Some therapies increase the risks of infections, and some may increase the risk of other autoimmune conditions. Others work more selectively on the intestines and have less risks.
Each treatment is different, so it is very important to talk with the health care team about specific risks and benefits of the treatment options. Before prescribing a biologic, the gastroenterologist will:
- Look at the medical history.
- Do a physical examination.
- Immunize against vaccine-preventable diseases, including hepatitis A and B viruses, shingles, influenza (annually), human papillomavirus, and pneumonia.
- Test for tuberculosis.
Routine follow-up care during treatment with blood tests and physical exam also helps to ensure safety. When prescribing biologics, the health care team will also think about how well the drug will work, how it is administered, the patient’s preferences and the cost of the medication.
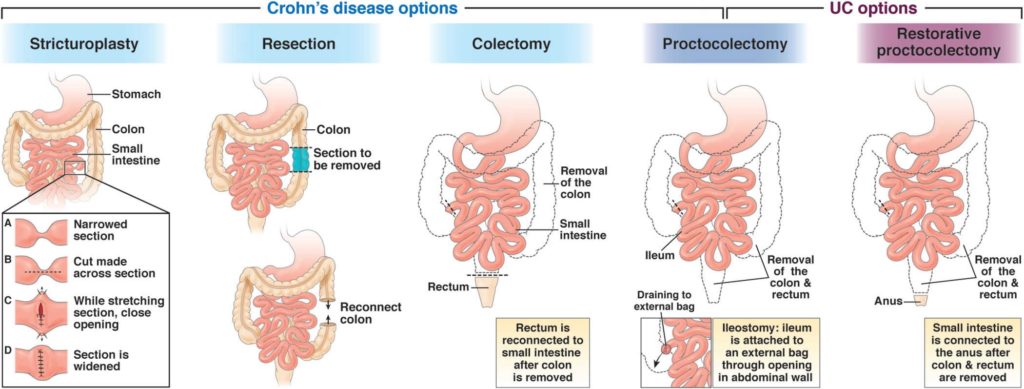
Surgery
Even with the availability of medicines to treat IBD, surgery may still be needed to manage IBD.
The options for surgery differ between UC and Crohn’s disease, and there are many types of surgery depending on the location of the disease in the intestines, the type of complication and the severity of the illness.
Options for patients with Crohn’s disease include:
Widens the bowel in the affected area.
Removes portions of the intestines. Once the affected intestine is removed, the two healthy ends of the intestine are joined back together (called anastomosis).
Removes the colon.
Removes the colon and rectum. Sometimes ileostomy is also done at this time, which is a procedure that brings the ileum, or end of the small intestine, through an opening in the abdominal wall to allow intestinal waste to drain out of the body. After the procedure, the patient wears an external bag over the opening to collect waste.
Surgery may be needed to remove abscesses (pus-filled mass) and fistulas if they are causing symptoms that do not respond to medication.
Options for patients with UC include:
Removes the colon and rectum. Sometimes ileostomy is also done at this time, which is a procedure that brings the ileum, or end of the small intestine, through an opening in the abdominal wall to allow intestinal waste to drain out of the body. After the procedure, the patient wears an external bag over the opening to collect waste.
Also known as ileoanal pouch anal anastomosis. Removes the colon and rectum but allows the patient to continue to pass stool through the anus.
Before having surgery for IBD, it is important to understand what the aim of the surgery is, what will happen during the procedure and the length of the recovery period.
Patients with IBD having surgery should speak to other patients who have had the procedure. Previous patients are often very willing to share their experiences and add perspective.
Complementary/alternative medicine
There are other types of treatments called complementary and alternative medicine (CAM).
The National Center for Complementary and Integrative Health defines CAM as a group of varied medical and health care systems, practices and products that are not looked at as part of conventional Western medicine. These may include changes in lifestyle, diet and nutrition, as well as the use of herbal treatments, vitamins and medical marijuana.
While scientific evidence is available for some CAM therapies, well-designed medical studies may still be needed to discover whether these treatments are safe and useful. Given possible side effects and interactions, patients should speak to their gastroenterologist about the benefits and limitations of CAM before using any type of CAM therapy.
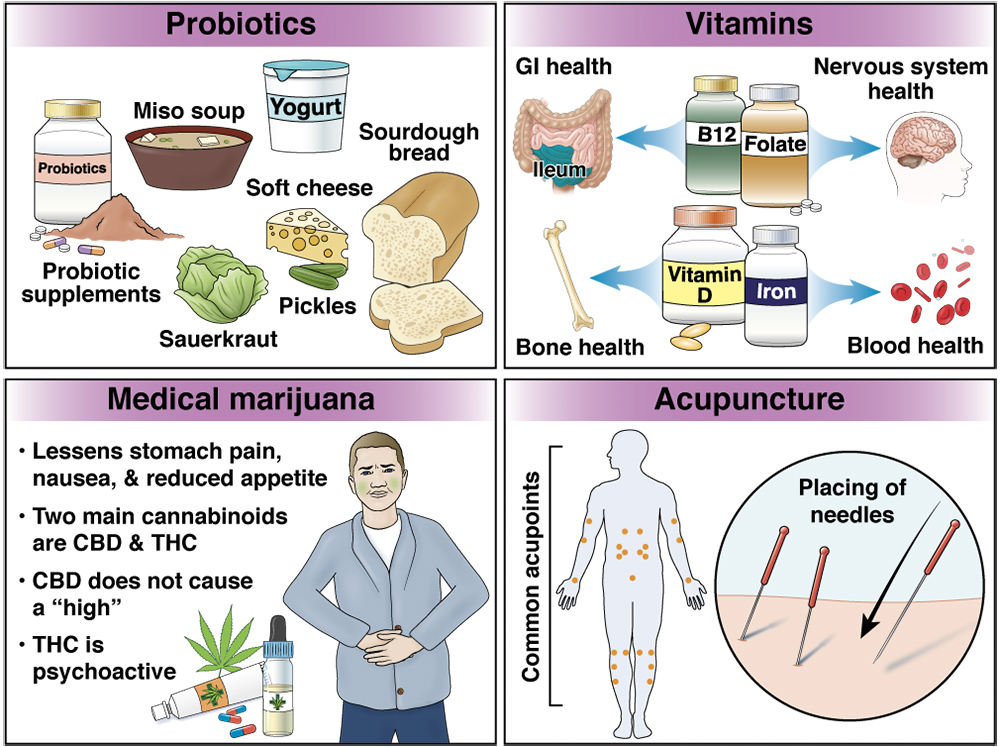
Vitamin or mineral deficiencies are common in people with IBD, so supplementation is sometimes needed.
- Vitamin B12 is absorbed in the lower section of the small intestine (ileum). People who have ileitis (Crohn’s disease that affects the ileum) or those who have undergone small bowel surgery might be deficient in (not have enough) vitamin B12. It is available as an oral supplement, a monthly injection into the muscle or as a once-weekly nasal spray.
- Vitamin D deficiency is common in people with Crohn’s disease. Vitamin D is important for strong bones and for helping the body use calcium. A daily vitamin D supplement is recommended for those with active bowel symptoms.
- Bone health: Certain medicines, such as glucocorticoids, may also have a negative effect on bone health. Long-term use of prednisone and other corticosteroids slows the creation of new bones and speeds up the breakdown of old bone. It also blocks the body from absorbing calcium.
- Iron: Iron deficiency, also known as anemia, is a result of blood loss from swelling and ulceration of the intestines. Patients with IBD can take an oral iron supplement.
- Folate is another B vitamin that is important for the nervous system and in making blood cells. It is particularly important to take enough before and during pregnancy.
Probiotics are among the most popular CAM therapies and come in many forms, including single or multiple strains of bacteria and/or yeast. Read more about probiotics here.
Medicinal formulations of marijuana are used by some patients with IBD that can include some formulations of cannabidiol (CBD), others that include tetrahydrocannabinol (THC), or others that include both CBD and THC or any of the other more than 100 known cannabinoids.
- CBD use has been found to lessen symptoms of stomach pain, nausea and reduced appetite, but it does not cause a “high.”
- THC is psychoactive and may have psychological effects.
Despite enthusiasm, more evidence is needed to confirm that the components of marijuana treat inflammation, so this must be used in combination with other treatments of IBD. It is important to know which states have medicinal marijuana laws and what is required for access.
Acupuncture is a Chinese therapy that has been used for thousands of years for many illnesses. Acupuncture is the practice of placing thin needles into the skin at certain acupoints to gain a desired benefit. Acupuncture may help abdominal pain, but it is not a proven treatment of inflammation.
Reviewed by

Esther A Torres
MD, AGAF
Professor of medicine, University of Puerto Rico School of Medicine, San Juan

Esther A Torres
MD, AGAF
Professor of medicine, University of Puerto Rico School of Medicine, San Juan