What is colonoscopy?
A colonoscopy is a test to look inside your colon. It is done by a gastroenterologist, a doctor trained in looking at the gastrointestinal (GI) tract.
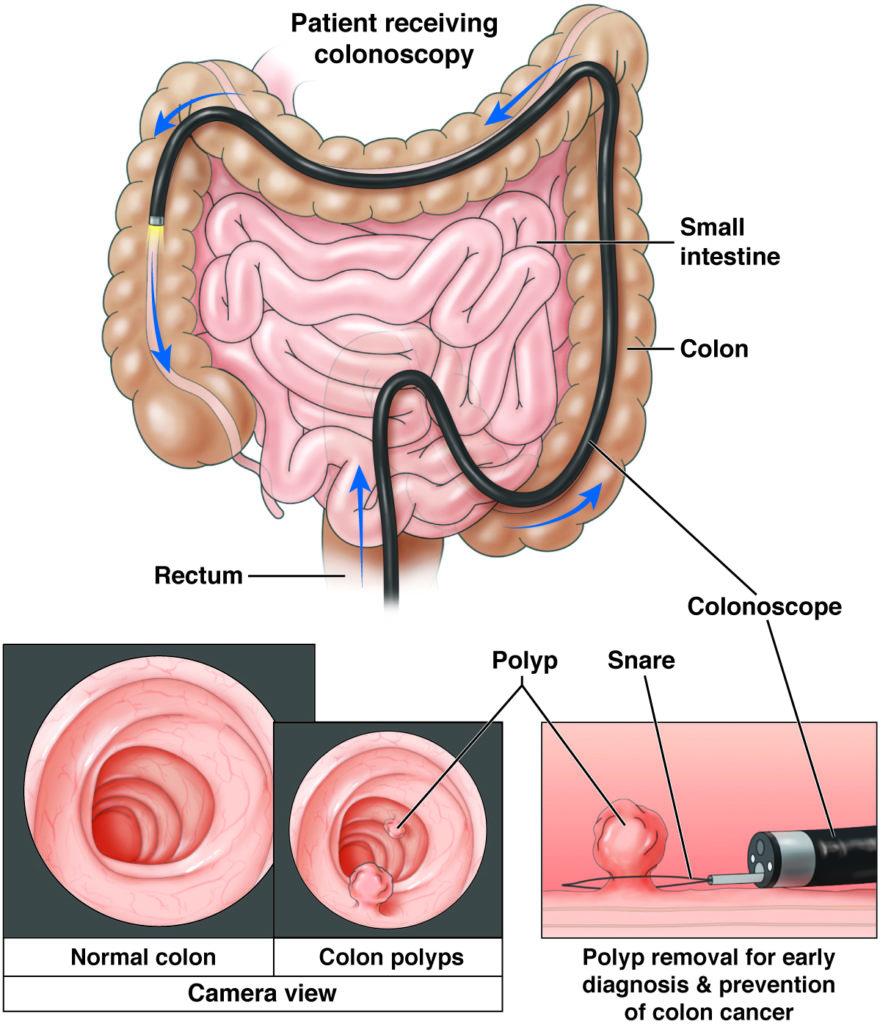
The main tool used to look inside the colon is a colonoscope. A colonoscope is a long, thin (about the width of your little finger), flexible tube with a tiny camera and a light on the end. It is long enough to look at all of the large bowel and even the lower part of the small intestine.
A colonoscopy is a safe and effective way to look for GI health issues and sometimes even treat those health issues.
It’s important to get a high-quality colonoscopy. Keep in mind that high cost doesn’t necessarily mean high quality.
Ask your doctor how often he or she reaches the end of the colon and how often he or she finds polyps.
A colonoscopy is the main way to check for diseases of the colon, such as colitis or cancer, and to remove colon polyps.
- A polyp is a mushroom-like growth on the inside wall of the colon or rectum.
- Polyps grow slowly over many years.
- Some polyps become cancerous, and others do not.
A colonoscopy is also a safe and helpful way to look at health issues in the gastrointestinal (GI) tract, such as
- Belly pain that won’t go away.
- Rectal pain that won’t go away.
- Blood in your stool.
- Change in bowel habits, such as diarrhea (loose stool), that won’t go away.
- Inflamed (swollen) colon that is seen on a computerized tomography (CT) scan.
During a colonoscopy, tools can be passed through the colonoscope to painlessly remove a suspicious-looking growth or to biopsy (take a small tissue sample).
The colon
The colon, or large intestine, is the last part of your digestive tract
It starts at the cecum, which attaches to the end of the small intestine.
The colon is made up of a hollow tube about five feet long that:
- Takes in water and minerals from digested food.
- Ends in the rectum, the last part of the large intestine, which stores undigested solid waste.
Colorectal cancer
Cancer of the colon and rectum — called colorectal cancer (CRC) — occurs when a growth on the lining of the colon or rectum has become cancerous.
CRC is the third most common cause of cancer in both men and women. It is the second-leading cause of cancer deaths in the U.S.
CRC can be prevented by finding colon and rectal polyps before they have the time to transform into colon or rectal cancer.
A colonoscopy can find and treat colon cancer
Colorectal cancer screening should start at age 45 for average-risk individuals.
Individuals at high risk should speak with their primary care provider or gastroenterologist about the appropriate age to initiate screening.
- Individuals at high risk include those with a family history of colorectal cancer or colorectal polyps, a personal history of hereditary polyposis syndromes, Crohn’s disease, ulcerative colitis, or prior abdominal radiation.
How to prepare for a colonoscopy
These are general instructions. Be sure to follow any instructions given to you by your doctor.
Your doctor or nurse will review the steps with you and make sure that you know how to get ready and what you can expect during and after the test. If you have any questions, be sure to bring them up with the doctor or nurse.
Give your doctor a list of all the medications you are taking and any allergies you have
- The list should include both prescription and over the counter (OTC) drugs, like aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), or vitamins or supplements.
- Ask your doctor before the test if any of your medications should be taken on the day of your colonoscopy.
- Ask your doctor before the test if any of your medications should not be taken before your colonoscopy.
- Ask your doctor before the test if you should take your medications the night before your colonoscopy.
Tell your doctor if you:
- Have diabetes and what medications you are on for it.
- Are taking blood thinners or have bleeding or blood-clotting problems.
- Have a pacemaker or other implanted electromedical devices.
- Have had stomach or bowel surgery, swallowing problems or other gastrointestinal (GI) problems.
- Have heart, lung or any other health problems that may need special care before the test.
Clean out your colon – a vital step
One vital step to get ready for your colonoscopy is to fully clean out the colon. For many, this step can be the hardest part of the colonoscopy.
You need to do this step carefully and completely, because if your colon is not cleaned out enough, your doctor will not be able to do a high-quality colonoscopy.
Many methods can be used to help cleanse the bowel, and your doctor will tell you which is best for you.
- Often, you will need to eat only clear liquids the day before the test.
- Often, you will need to drink a liquid (a laxative) that will help you move your bowels until your stool comes out clear. If your doctor tells you to drink this, be sure to drink it all.
- Other ways to clean out your bowels involve different special diets or the use of enemas or suppositories.
Whichever method or blend of methods is suggested for you, be sure to follow your doctor’s orders as directed.
Important!
- Check your instructions about what to eat or drink the night before your colonoscopy and when to stop eating and drinking.
- Since you will be given medicine to block pain and make you feel sleepy during the colonoscopy, you will not be allowed to drive a car, work or make important decisions after the test.
- You must have someone with you to review the discharge instructions and to drive you home after the test.
- Plan to rest at home for the rest of the day after your test.
A colonoscopy can be done as an outpatient procedure in your doctor’s office, outpatient surgical center or hospital. Be sure you know exactly where you need to go the day of your procedure, as it may not be the same as your doctor’s office.
Be sure to ask your doctor or nurse if there is anything you do not understand.
Day of your colonoscopy
Your doctor will tell you more specifically what you can expect during the test. Some things may include:
- A nurse will review your medical history, medications and allergies.
- You will change into a hospital gown.
- Your doctor will review the consent form for the test, answer any of your questions and ask you to sign the form, which says you understand the test being done.
- An intravenous (IV) line will be started (to give you IV fluids and medicine to make you feel sleepy during the exam).
During your colonoscopy
You will be given medicine to block pain and make you relaxed and sleepy (or totally asleep), so you won’t feel much during the colonoscopy.
During the test, everything will be done to make sure that you are at ease, safe and comfortable.
Once you are fully relaxed, the doctor will do a rectal exam with a gloved, lubricated finger. Next, the lubricated colonoscope will be gently and carefully placed into your rectum, passing through the anus. Generally, it will not hurt.
The doctor will then use a colonoscope (a long, thin [about the width of your little finger], flexible tube with a tiny camera and light on the end) to be able to see inside.
- The colonoscope is long enough to look at all of the large bowel and even the lower part of the small bowel.
- Your doctor will put it in as far as it can go without hurting you.
- Air will be passed through the colonoscope to expand the bowels so that the doctor can see better. You may feel the need to move your bowels or some cramping or fullness.
In some cases, the doctor may need to do a biopsy (taking a small piece of tissue to look at under the microscope). You will not feel this.
The time it takes to do a colonoscopy varies, based in part on what is found and what is done. If a polyp is found, your doctor will usually remove it using tools in the colonoscope. This will take more time.
After the doctor is done looking inside, the endoscope will be removed and you will wake up in recovery as the medicine wears off.
After your colonoscopy
Your doctor will tell you more specifically what you can expect after the test. Some things may include:
- When your colonoscopy is done, you will be cared for in a recovery room until the medicine wears off and you are more alert.
- Your doctor or nurse will review the colonoscopy results with you and give you any other details or next steps you may need.
- If a biopsy (taking a small piece of tissue to look at under the microscope) was taken, your doctor or nurse will tell you when those results will be available. They will tell you if any other testing or follow-up is needed.
- You will be told how soon you can eat and drink, plus other steps to take for getting back to your normal routine.
- Plan to take it easy for the rest of the day after your colonoscopy. This means not driving, working or making important decisions.
- You will need to arrange to have a family member or friend with you who can hear the discharge instructions and take you home. You should plan to resume your normal activities (driving and working) the day after your test.
Possible minor issues
- You may feel some minor issues, such as bloating (swelling), gas or mild cramps right after the test. These should go away in less than 24 hours.
- Contact your doctor’s office if you have any questions after your colonoscopy.
Colonoscopy safety
Although colonoscopy is a safe test, complications can happen sometimes. Problems during a colonoscopy are rare.
Some examples may be:
- Tearing or puncturing of the colon walls, which could call for emergency surgery to fix.
- When a polyp is taken out or a biopsy (taking a small piece of tissue to look at under a microscope) is done, it could result in heavy bleeding. Sometimes a blood transfusion is needed. Sometimes the colonoscope needs to be put back in to control the bleeding.
You should know that colonoscopy is not perfect and even with a skilled doctor, some colon lesions (abnormalities) might be missed.
Be sure to talk with your doctor about any specific concerns you have about the test.
Reviewed by

Folasade (Fola) Popoola May
MD, PhD, MPhil,
Assistant professor of medicine, University of California, Los Angeles (UCLA), Health
November 2024

Folasade (Fola) Popoola May
MD, PhD, MPhil,
Assistant professor of medicine, University of California, Los Angeles (UCLA), Health
February 2021