What is colorectal cancer?
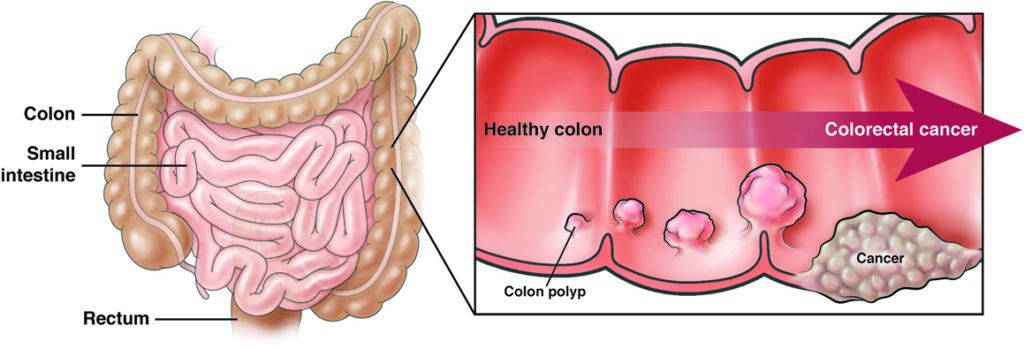
Colorectal cancer (also known as colon cancer) is cancer of the colon and/or rectum and occurs when a growth in the lining of the colon or rectum becomes cancerous.
The colon is a vital organ in your body’s digestive system. The rectum is the very end of the colon. The colon and rectum, known as the large intestine, is a long, thick tube that:
- Takes in water and minerals from digested food.
- Stores undigested solid waste.
Most colorectal cancers come from precancerous polyps — adenomatous polyps or serrated polyps — that form over a number of years (5 to 10) to become a cancer. A polyp is a mushroom-like or flat growth on the inside wall of the colon or rectum. Polyps grow slowly over many years.
Not all colon polyps have the same risk of turning into colon cancer. Precancerous polyps could become cancerous; other types of polyps (hyperplastic, inflammatory) do not.
Who gets colorectal cancer?
As of 2020, colorectal cancer is the 3rd-most common cause of cancer in both men and women. It is the 2nd-leading cause of cancer deaths in the U.S. While men and women have the same lifetime risk for CRC, men are at higher risk than women at any given age.
Black individuals and American Indians/Native Americans are more likely to be diagnosed with colorectal cancer and more likely to die from colorectal cancer than White Americans.
Colon and rectal polyps can occur at any age but are most common after age 45.
Colorectal cancer rates are highest in adults over age 50; however, since the 1990s, colorectal cancer rates have increased in individuals aged 49 and younger.
To lower the chance of colorectal cancer, it is vital to get screened at the right time.
* If you are at average risk, start screening at age 45.
* If you have a family history of colorectal cancer or polyps, start screening at age 40 or at the age that is 10 years younger than the earliest member of your family was diagnosed with colorectal cancer or polyps, whichever is earlier.
* Individuals with inflammatory bowel disease (IBD, Crohn’s disease or ulcerative colitis), or a history of abdominal radiation should discuss the appropriate time to initiate screening with their providers.
* If you think you might be at high risk for colorectal cancer, talk to your doctor early, before age 45, to make a screening plan that’s right for you.
Colon cancer screening can save your life
- Colorectal cancer screening is safe, effective, and recommended for all adults.
- With routine colorectal cancer screening, more than 1/3 of colorectal cancer deaths can be avoided.
- Many tests can help find precancerous and cancerous growths. Finding them early could save your life.
- Finding and getting rid of colon polyps prevents colon cancer, no matter what your risk is.
- Begin talking with your primary care provider or gastroenterologist about CRC screening at age 45 to discuss screening options and insurance coverage.
- With simple steps, you can lower your risk of getting the disease.
Check out AGA’s informative videos on colorectal cancer screening
Symptoms
Colorectal cancer does not cause symptoms early, which is why routine screening is essential.
As colorectal cancer progresses, there are a number of symptoms or warning signs that can happen, such as:
- Rectal bleeding.
- Blood in your stool (bright red, black or very dark).
- Temporary change in your bowel movements, especially in the shape of the stool (e.g., thin like a pencil).
- Pain in having a bowel movement or the urge to move your bowels without having a bowel movement.
- Frequent cramping pain in your lower belly.
- Frequent gas pains.
- Weight loss without dieting.
I feel fine. Why not wait for these symptoms to develop, rather than have a colonoscopy?
-
Precancerous polyps often do not cause symptoms and removing them can prevent colorectal cancer.
-
Early colorectal cancer does not always cause symptoms.
-
Colorectal cancers found in people without symptoms are not as advanced and more frequently cured.
-
Detection of colorectal cancers at an early stage increases your chance of cure and survival.
-
There are more treatment options when colorectal cancer is diagnosed at an early state.
What should I do if I have these symptoms?
If you are having any of the above symptoms, call your gastroenterologist or primary care physician right away. He or she will ask questions about your symptoms and figure out the best diagnostic test for you.
Risk factors
You may be at normal or greater risk for colorectal cancer, based on your age, race, personal medical history and family medical history.
Increased risk
You are considered to be at increased risk for colorectal cancer if you have a family history of colorectal cancer or polyps, a hereditary polyposis syndrome, Crohn’s disease or ulcerative colitis. Black individuals are also at increased risk. People in these groups should talk to their primary care provider or gastroenterologist about the appropriate age to begin colorectal cancer screening.
Average risk
You are considered average risk for colorectal cancer if you are age 45 or older and have none of these risk factors:
- Have had colorectal cancer or precancerous polyps before.
- Have had one or more parent, brother or sister, or child who has had colorectal cancer or polyps.
- Have had family members with cancers, such as colorectal cancer or cancer in the uterus, ovary or other organs.
- You identify as Black American/African American.
- Have (or have had) IBD, such as ulcerative colitis or Crohn’s disease.
- Have Lynch syndrome (hereditary non-polyposis colon cancer), which does not have a large number of polyps as a warning sign but often involves a family history of colorectal cancer among multiple family members in many generations
- Have a hereditary polyposis syndrome, such as familial adenomatous polyposis (FAP), which leads to hundreds of polyps in the colon or rectum during the teen years; often one of these grows into cancer by age 30.
Talk to your doctor about your risk factors and when it is best to start screening.
Colorectal cancer screening options
Questions to ask your doctor
1. What are my CRC screening test options given my personal and family medical history?
2. What are the risks and benefits of each option?
3. What happens if a polyp is found?
4. How do I get ready for my test?
5. How often should I be tested if my colon is clear?
6. If a polyp is found, when should I get tested again?
7. How often do you perform each test?
8. How often do you need to do a standard colonoscopy after doing a different test first?
How to prevent colon cancer
Along with getting tested regularly, healthy life choices are usually recommended as the best way to lower your risk of colorectal cancer.
Here’s how you can help lower your risk
- Do not smoke or use tobacco products.
- Eat more foods that are high in fiber, such as whole grains, fruits and veggies.
- Eat more cruciferous veggies, such as cabbage, broccoli, cauliflower and brussels sprouts.
- Raise calcium intake with low-fat milk, shellfish, salmon and calcium supplements with vitamin D.
- Eat less fats, oils, butter and red meat.
- Limit your intake of charcoal-broiled foods, and skip salt-cured foods.
- Limit your intake of highly processed foods.
- Get active.
- Keep your weight in the normal range.
- Limit alcohol intake.
Reviewed by

Folasade (Fola) Popoola May
MD, PhD, MPhil
Assistant professor of medicine, University of California, Los Angeles (UCLA), Health

Folasade (Fola) Popoola May
MD, PhD, MPhil
Assistant Professor of Medicine, University of California, Los Angeles (UCLA), Health