What is ERCP?
ERCP stands for
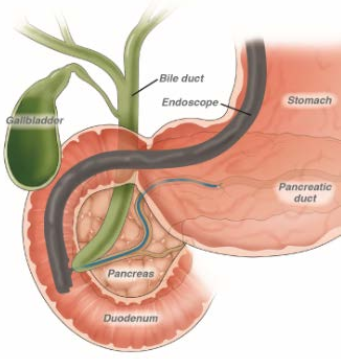
- Endoscopic — Refers to a tool called an endoscope, a long, thin (about the width of your little finger), flexible tube with a camera on the end.
- Retrograde — Refers to the direction (backward) in which the endoscope injects a liquid for X-rays of parts of the GI tract called the bile duct system and pancreas.
- Cholangio — Refers to the bile duct system.
- Pancreato — Refers to the pancreas
- Graphy — Refers to taking pictures (x-rays).
The endoscope used in ERCP is a duodenoscope.
A duodenoscope is a long, thin, flexible and lighted tube that is advanced by the physician passed through the mouth, throat and stomach, and into the small intestine (duodenum). The duodenoscope has a part at the end called an “elevator channel” which allows the physician to manipulate devices. In the U.S., duodenoscopes are used in more than 650,000 ERCP procedures each year.
Using tools passed through the duodenoscope, your doctor can inject dye to light up organs under X-rays. This provides a clear view of your pancreas, pancreatic duct, bile duct system, gallbladder and duodenum (the first portion of the small intestine).
ERCP is an endoscopic procedure used to inject dye into the bile and pancreas ducts. X-ray pictures are then taken.
Conditions ERCP can detect and/or treat
ERCP can help find the cause of jaundice (when your skin and/or the whites of your eyes turn yellow) or pancreatitis, which is inflammation (swelling and redness) of the pancreas that is often caused by gallstones or alcohol abuse. ERCP can also treat some of those issues.
ERCP can see if there is a blockage or narrowing in your biliary or pancreatic ducts caused by stones, tumors or scarring.
ERCP is frequently performed to find the cause of abnormal liver-chemistry tests and to follow up on an abnormal ultrasound, CT scan or MRI exam.
During an ERCP, if any blocks are found, tools can be passed through to relieve the block. Stones can be removed from the common bile duct or pancreatic duct and blocks can be dilated, biopsied and/or stented.
ERCP can relieve jaundice (when your skin and/or the whites of your eyes turn yellow) caused by blocked bile ducts.
ERCP can help find the cause of pancreatitis, inflammation (swelling and redness) of the pancreas, and prevent future attacks.
ERCP may help you avoid surgery in some cases.
Preparing for ERCP
Give your doctor a list of all the medications you are taking and any allergies you have.
- The list should include both prescription and over-the-counter (OTC) drugs, like aspirin, NSAIDs, or vitamins and supplements.
- Ask your doctor before the test if any of your medications can be taken on the day of your ERCP.
- Ask your doctor before the test if any of your medications should not be taken before your ERCP.
- Ask your doctor before the test if you should take your medications the night before your ERCP.
Tell your doctor if you:
- Have diabetes and what medications you are on for it.
- Are taking blood thinners or have bleeding or blood-clotting problems.
- Have a pacemaker or other implanted electromedical devices.
- Have had stomach or bowel surgery, swallowing problems or other gastrointestinal (GI) problems.
- Have heart, lung or any other health problems that may need special care before the test.
Do not eat or drink anything for at least six hours before the test. If it is scheduled for first thing in the morning, do not eat or drink anything after midnight. If you do not remember the time of your appointment, call your doctor.
Since you will be given medicine to block pain and make you feel sleepy (sedation), do not drive a car, work or make important decisions after the test. Most patients resume their normal activities the following day. Your doctor can provide specific instructions.
You must have someone with you to review the discharge instructions and to drive you home after the test.
Plan to rest at home for the rest of the day after your test.
ERCP can be done as an outpatient procedure, but some people may need to go to a hospital based on their individual cases. Be sure you know exactly where you need to go the day of your procedure as it may not be at your doctor’s office. Ask your doctor or nurse if there is anything you do not understand.
During your ERCP
- A nurse will review your medical history, medications and allergies.
- You will change into a hospital gown.
- Your doctor will review the consent form for the test, answer any of your questions and ask you to sign the form, which says you understand the test being done.
- An intravenous (IV) line will be started to give you fluids and medicine to make you feel sleepy during the exam.
What to expect
You will be given medicine to block pain and make you relaxed and sleepy, so you won’t feel much during the ERCP.
During the test, everything will be done to make sure that you are at ease, safe and comfortable. You may feel full during the test, since air may be put in to help move the scope.
Your blood pressure, pulse and the oxygen level in your blood will be monitored during the test.
You may have the back of your throat sprayed with something to numb it to lessen discomfort of the endoscope.
A plastic bite block may be placed between your teeth (to protect your teeth and the endoscope).
Once you are fully relaxed, the endoscope will be carefully passed through your mouth, into your esophagus (tube that links your mouth and your stomach) and into your stomach and duodenum, the first section of your small intestine.
The doctor will use an endoscope (a long, thin [about the width of your little finger], flexible tube with a tiny camera and light on the end) to be able to see inside. The endoscope will not block your breathing.
In some cases, the doctor may need to do a biopsy (taking a small piece of tissue to look at under a microscope). You will not feel this.
In the duodenum, a smaller tube is put down through the endoscope and can be led into either the pancreatic or common bile duct (based on where your issue is). This smaller tube puts a special dye into the ducts.
X-ray machines are then used to take pictures of the dye lighting up the ducts. This way, widening, narrowing or a block of the ducts can be seen.
Some of the problems that may be seen during an ERCP can also be treated at the same time.
- If a stone is causing a block, your doctor is often able to remove it.
- Your doctor may do a sphincterotomy, which opens the entry of the ducts into the bowel.
- A small camera may be passed into the bile or pancreatic duct to visualize and photograph stones, strictures or tumors, and to facilitate biopsies or break up large stones.
- A stent (small, plastic or metallic, mesh tube) can be put in your ducts if they are obstructed or constricted.
After the doctor is done looking inside, the endoscope will be removed, and you will wake up in recovery as the medicine wears off.
After ERCP
- When your ERCP is done, you will be cared for in a recovery room until the medicine wears off and you are more alert.
- Plan to take it easy for the rest of the day after your ERCP. This means not driving, working or making important decisions.
- You will need to arrange to have a family member or friend accompany you to the appointment so that he or she can hear the discharge instructions and take you home. You should plan to resume your normal activities (driving and working) the day following your exam.
- You may feel some minor issues, such as bloating (swelling) or feeling full. You may pass a lot of gas right after the test. You may have soft stool or other brief changes in your stool after the ERCP. These should go away in less than 24 hours.
- Your doctor or nurse will review the ERCP results with you and give you any other details or next steps you may need.
- If a biopsy (taking a small piece of tissue to look at under a microscope) was taken, your doctor or nurse will tell you when those results will be available. They will tell you if any other testing or follow-up is needed.
- You will be told how soon you can eat and drink, plus other steps to take for getting back to your normal routine.
Contact your doctor’s office if you have any questions after your ERCP.
Safety of ERCP
Be sure to talk to your doctor about your risk and any concerns you may have.
Depending on your case, ERCP can have may have a 5 to 10 percent risk of complications or adverse events. In rare cases, severe complications may call for hospitalization.
Mild to severe inflammation (swelling) of the pancreas can happen. This is known as acute pancreatitis. You can ask your doctor if they can give any medication to reduce this risk. You may need go to hospital for treatment. You may need surgery.
Bleeding can happen in an ERCP, especially if a sphincterotomy is performed. This bleeding usually stops on its own.
A puncture or tear of the bowel wall or bile duct is a rare problem that can happen.
Infection can happen. Treatment for infection is antibiotics and restoring drainage if there is a block. There have been reports of antibiotic-resistant infections that come from the endoscope tool used. The FDA has worked with endoscope manufacturers and provided strict guidelines for cleaning and disinfection to minimize this risk. Talk to your doctor about any concerns on this issue.
You may have an allergic reaction to any of the medications used during ERCP, but these are mostly minor.
If you have any of these symptoms after your ERCP, call your doctor right away.
- Severe pain in your upper abdomen and/or back area. that isn’t helped by pain medicine.
- Severe nausea.
- Vomiting.
- Trouble swallowing.
- Bloody, black or tarry stool.
- Chills or fever over 100 degrees Fahrenheit.