What is the low-FODMAP diet?
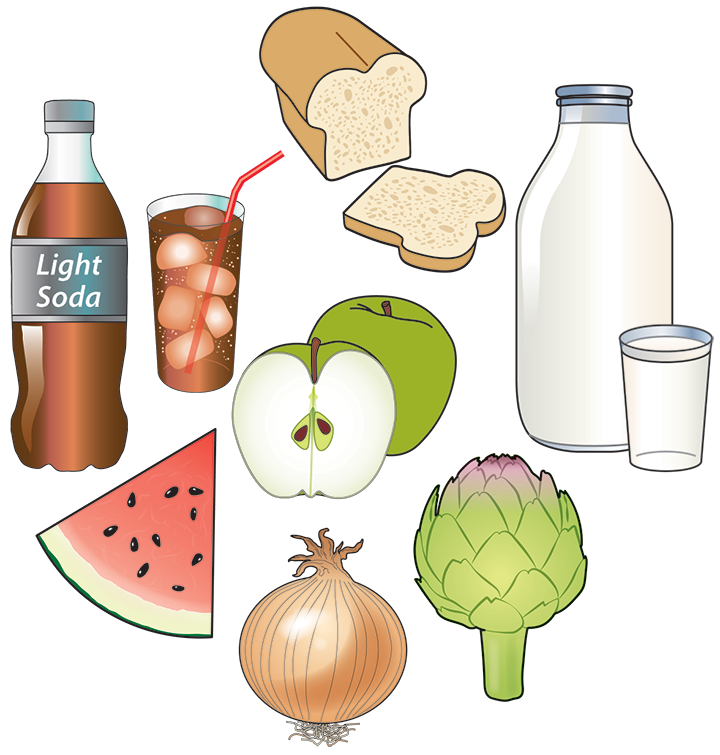
A low-FODMAP diet contains a limited amount of FODMAPs. FODMAPs are found in some carbohydrates and fibers that are in many common foods, including the example foods shown below. When you eat foods that have FODMAPs, the normal gut bacteria use these as fuel (ferment) and this can also pull water into your intestines. If you have a sensitive gut, you might have digestive distress after eating more FODMAPs than you can handle.
A low-FODMAP diet may be recommended to help you figure out how food choices and portion sizes can help you manage your symptoms. This is only one part of the diet.
FODMAP stands for:
- Fermentable: creates gas
- Oligosaccharides: specific types of fiber found in beans, onion, wheat and garlic
- Disaccharide: lactose (or milk sugar) found in milk, yogurt and ice cream
- Monosaccharide: excess fructose, found in mango, apples, pears and watermelon
- And
- Polyols: a group of sugar alcohols sometimes used to sweeten sugar-free gum and mints, and found naturally in pears, plums, nectarines, and cauliflower
Gluten and dairy are not FODMAPs. A low-FODMAP diet is not gluten-free or dairy-free.
What symptoms can low-FODMAP diet help?
Symptoms that might improve on a low-FODMAP diet include:
- Bloating
- Belly pain
- Too much gas
- Diarrhea (loose or watery stool 3 or more times a day)
- Constipation (hard-to-pass bowel movements [stool] less than 3 times a week)
What conditions are the low-FODMAP diet used for?
- Irritable bowel syndrome (IBS)
- Inflammatory bowel disease (IBD, Crohn’s disease or ulcerative colitis) with symptoms that aren’t going away, despite being in remission (time when you feel well).
- Celiac disease with ongoing symptoms despite a 100% gluten-free diet.
A low-FODMAP diet may help improve symptoms related to these conditions, but it is not a cure. It shouldn’t be used for any other reason. Low-FODMAP is not a weight loss diet.
How to start a low-FODMAP diet
Low-FODMAP diets can be used in two ways:
1. Make a few simple changes to lower your intake of FODMAPs, such as:
- Use lactose-free milk products.
- Drink water instead of sweetened beverages and fruit juices.
- Cut way back on onions and garlic.
- Choose oranges, grapes or pineapple instead of apples.
Ask a dietitian to point out the highest FODMAP foods and beverages you are consuming and suggest some lower FODMAP options.
2. If you don’t have too many other dietary restrictions and your health care provider or dietitian says it is safe for you to do so, you can try a three-step process.
- Elimination (avoiding high-FODMAP foods for 2-4 weeks to see if it helps).
- Reintroduction (adding FODMAPs back to your diet to see which ones are well tolerated and which are symptom triggers).
- Personalization (returning to the most varied diet that you can comfortably enjoy).
Be sure to tell your health care provider if you have ever had an eating disorder or if you are feeling afraid of food or eating. The three-phase process is not usually recommended in such cases.
Resources
Written by
Patsy Catsos, MS, RDN, LD, and Kate Scarlata, MPH, RDN
Reviewed by the DIGID Disorders of the Brain Gut Interaction workgroup ©March 2021
Patsy Catsos, MS, RDN, LD, and Kate Scarlata, MPH, RDN
Reviewed by the DIGID Disorders of the Brain Gut Interaction workgroup ©March 2021