What is fecal microbiota transplantation (FMT)?
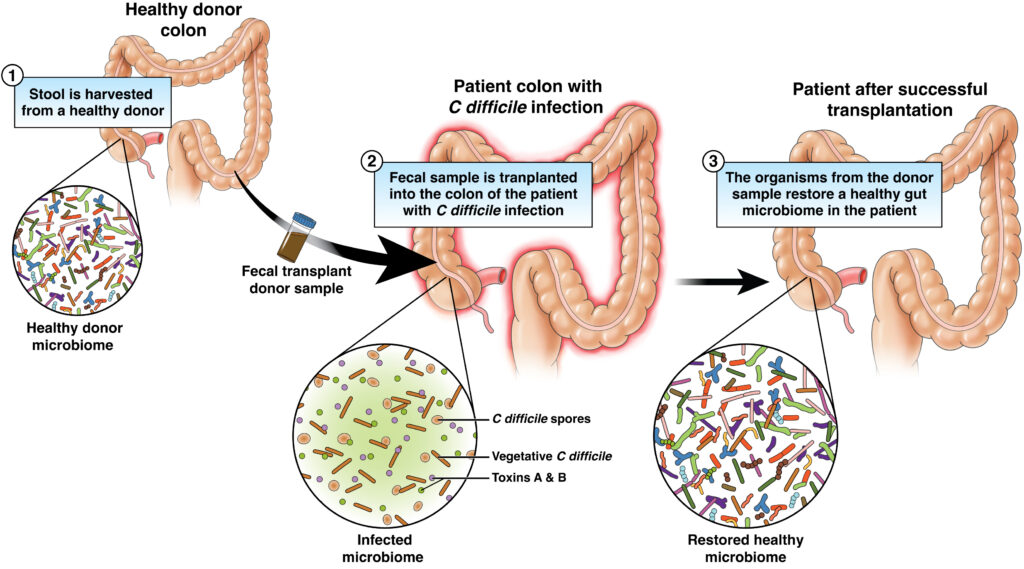
Fecal microbiota transplantation (FMT) is when stool from a healthy donor is made into a liquid mixture and transferred into the colon of a different person to reintroduce helpful organisms.
FMT is primarily used to treat Clostridioides difficile (C. diff) infection that has occurred many times despite adequate antibiotic treatment. FMT is considered a success if the person with C. diff has no relapses for eight weeks. Research shows that FMT has a high success rate, though some people with stubborn C. diff may require more than one transplant.
There is ongoing research to find out if FMT may work for other health issues.
C. diff may impact certain groups of the population differently. C. diff infection is more likely to affect White patients than patients from any other ethnic group, but Black patients are more likely to have increased severity of disease and mortality.
Be part of the AGA FMT National Registry
If you are considering FMT, ask your health care provider if they participate in the American Gastroenterological Association (AGA) FMT National Registry data collection project. Our goal is to track 4,000 patients for 10 years. The data we collect will allow us to identify potential short-term adverse outcomes and to search for long-term safety concerns, such as development of chronic conditions like irritable bowel syndrome (IBS), obesity and diabetes. Learn more about how to contribute to advancing the future of FMT.
Who can get FMT?
FMT may be an option for people who have had:
- At least three episodes of mild to moderate C. diff infection that have not responded to standard antibiotic therapy and have had recurrent symptoms after six to eight weeks of treatment with antibiotics.
- At least two episodes of severe C. diff infection that required them to be admitted to the hospital.
- Severe C. diff infection or severe colitis caused by C. diff that did not respond to antibiotics within two days.
Not everyone is a good candidate for FMT. The procedure can be risky for people who are taking drugs that suppress their immune system, have had a recent bone marrow transplant, or have cirrhosis of the liver or advanced HIV or AIDS. If you fall into one of these groups, your doctor may urge against it, based on how bad your C. diff infection is and whether you have other problems.
The impact of the COVID-19 pandemic
The COVID-19 pandemic has impacted the access to FMT due to the documented presence of viral particles in stool, that is of unclear clinical significance. In mid 2020, the FDA recalled all stool products from available stool banks severely restricting availability of donor stool to many centers and medical offices that were performing FMT.
Stool donors for FMT
There are strict standards to become a stool donor.
- Donors must be screened carefully to avoid transmitting dangerous viruses or bacteria to the person with C. diff.
- Doctors first screen potential donors by asking them the same questions they would ask of potential blood donors.
- Donors will also be tested for diseases that can be spread through the blood, such as hepatitis, HIV and syphilis.
- Donor stool will also be extensively tested for organisms that can spread in the stool, such as C. diff, parasites and other organisms.
- Since the COVID-19 pandemic, donors should be tested for COVID-19 at the time of their stool donation.
- People who have taken antibiotics within the last three months or who have diseases or conditions of the GI tract, such as IBS or chronic constipation, should not be donors.
Testing of the donor stool may not be covered by health insurance and can cost more than $500. Donors should check with their insurance companies and make a plan.
FMT procedures
Doctors use different techniques to do FMT, such as colonoscopy, enema, or infusion through an upper endoscope or nasogastric tube (NG tube; a tube the runs from your nose down into your stomach).
Each of these methods has some risk.
- For colonoscopy and enema, there is a very low risk of bowel perforation (a tear or hole in the bowel).
- For transfer using an NG tube, there is a small chance that some of the fluid holding the stool could end up in the lungs and cause an infection there.
Oral capsules are currently not widely available due to the COVID-19 pandemic.
Note
Though the procedures for FMT will depend on the health of the recipient and the preferences of the doctor doing the transplant, there are many things recipients and donors will have to do to get ready. Because the long-term results of FMT are not known, the U.S. Food and Drug Administration (FDA) needs an informed-consent form signed by the recipient.
Preparing for FMT
There are steps for recipients of FMT and stool donors.
Ideally, people who are going to get FMT should have an empty GI tract. Often, this means drinking only clear fluids and not eating solid food for 24 hours before the procedure.
People with mild or moderate C. diff may also be asked to drink a liquid that will make them move their bowels until their whole digestive system is empty. However, those with severe infection, colitis, pseudomembranous colitis (infection in the colon; overgrowth of C. diff bacteria), or toxic megacolon (widening of the colon; complication of inflammatory bowel disease [IBD] or infection of the colon) should not drink these preparations.
Recipients who will get the transplant by enema or colonoscopy may be given loperamide (Imodium®) the day of the procedure. This drug slows down the muscle that squeezes the intestines and colon so that the donor stool stays in the body longer and the helpful organisms in the stool have a better chance to have a good effect.
If the transplant is to be delivered by an NG tube, the recipient will be given a drug to stop the stomach from producing acid. The acid can potentially kill the helpful organisms in the donor stool.
Donors should avoid any foods that the recipient is allergic to for five days before the transplant. This will give the donor’s body time to clear the food from the GI tract.
Donors who have any sign of infection, such as fever, diarrhea (loose stool) or throwing up, between the time they are screened and the time of their donation should call the doctor who will be doing the transplant right away.
Your doctor may tell you to take a certain type of laxative that increases the amount of water in the bowel the night before the procedure. It will make passing a stool easier in the morning.
Reviewed by

Maria I. Vazquez Roque, MD, MS
Associate professor, division of gastroenterology and hepatology, Mayo Clinic, Jacksonville, Florida
Maria I. Vazquez Roque, MD, MS
Assistant professor, division of gastroenterology and hepatology, Mayo Clinic, Jacksonville, Florida