What are hemorrhoids?
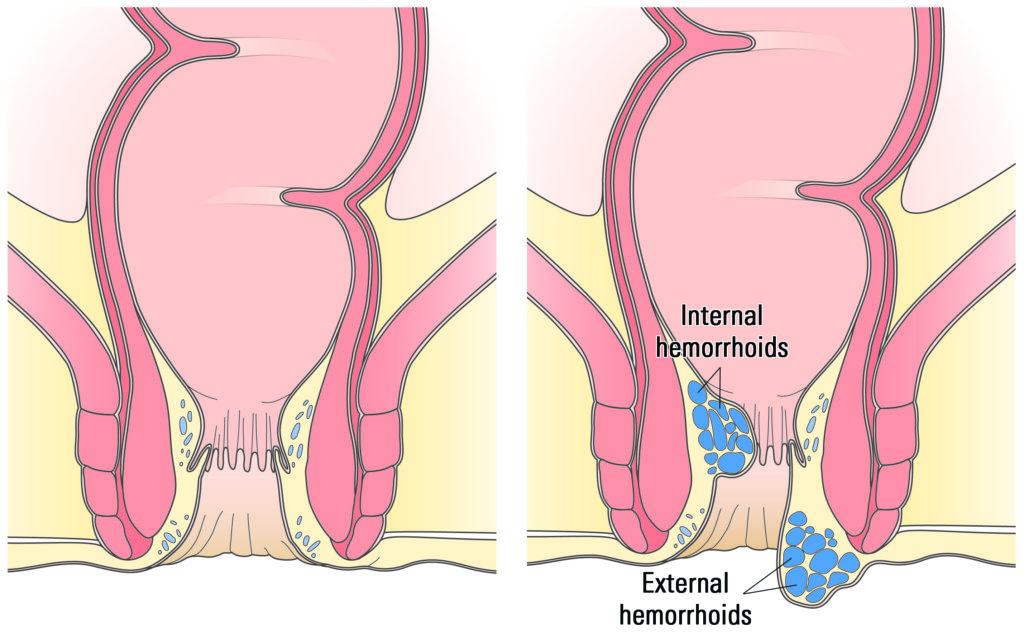
Each of us has veins around the anus that tend to stretch under pressure. When these veins swell and bulge, they are called hemorrhoids (or piles). One set of veins is inside the rectum (internal), and another is under the skin around the anus (external).
Hemorrhoidal tissue is thought to be helpful in holding back stool when we are at rest and in cushioning muscles when we move our bowels.
Swelling can be caused by straining to move your bowels, sitting too long on the toilet, or other causes, such as pregnancy, obesity or liver disease.
How common are hemorrhoids?
Hemorrhoids are very common in men and women. About half of all people have noticeable hemorrhoids by the age of 50. Many people have occasional bleeding from hemorrhoids.
Women’s problems may start during pregnancy. The pressure of the fetus in the abdomen, as well as hormonal changes, cause hemorrhoidal veins to swell. These veins also are placed under severe pressure during the birth of the baby. For most women, such hemorrhoids don’t last long.
Hemorrhoids are more common in obese individuals.
Symptoms of hemorrhoids
Internal hemorrhoids
- Often cause painless rectal bleeding.
- Cause bright red blood in stool, on toilet paper or in the toilet bowl.
- Bleeding happens when the swollen veins are scratched or broken by straining or rubbing.
- Medicines that thin the blood can make bleeding worse.
- An internal hemorrhoid may come through the anus and become swollen and painful.
External hemorrhoids
- Cause pain and discomfort around the anus.
- Cause painful swelling or a hard lump around the anus. This happens when a blood clot forms.
The symptom cycle
Swelling around the anus can cause bleeding and/or itching, which may start a vicious cycle of symptoms. Draining mucus or stool residue may cause itching. This can be caused by either too much rubbing or cleaning around the anus or poor cleaning habits with residual stool around the anus.
Did you know?
When many people think of hemorrhoids, they often speak of external hemorrhoids, but internal hemorrhoids, anal fissures (painful bowel movements due to a small cut in the anus) and other less common anal conditions can all cause bleeding, pain and itching around the anus.
Talk to your doctor if you don’t feel better after trying over-the-counter products.
Treatment of hemorrhoids
If your hemorrhoids do not go away or if you see blood in your stool, tell your doctor right away.
A doctor may:
- Look at your anus and feel the inside of the rectum with a gloved finger.
- Place a small tool into the rectum to see hemorrhoids. This is called an anoscopy.
- Look at the anal canal and colon with a flexible scope (colonoscopy or sigmoidoscopy). This is needed when internal hemorrhoids cannot be felt with a finger.
More fiber
Softer stools make it easier to move your bowels and lessen pressure on the veins. You may need to increase the fiber in your diet.
Eat more fresh fruits, leafy veggies, and whole-grain breads and cereals (especially bran).
Drink six to eight glasses of fluid (not alcohol) each day.
Your doctor may suggest that you use a supplement that gives you more fiber and softens the stool.
Good hygiene
Cleaning well after you have a bowel movement can help treat and prevent hemorrhoids.
- Bathe the anus gently after each bowel movement using soft, moist toilet paper.
- Avoid a lot of wiping. If needed, you can even use a bath or shower instead of wiping.
- After bathing, dry the anus gently with a soft cloth or towel.
To protect against irritation, cleanse the anus gently and apply a zinc oxide paste (or powder) to the area.
Medicated suppositories or creams can be found at the drugstore but are mostly meant for external hemorrhoids.
You can also try cold packs, a tub bath, warm soaks (a sitz bath) or bed rest to help calm pain or swelling.
Any of these home treatments may help the symptoms, and no other treatment may be needed. If symptoms do not go away, see your doctor.
Procedural treatments
In some cases, internal hemorrhoids that have fallen outside of the anus (prolapsed) or that bleed too much must be removed. Your gastroenterologist may be able to treat them during an outpatient visit to the office or to the hospital.
Many methods can be used to remove or reduce the number of hemorrhoids. Talk to your doctor about recovery and which option is best for you.
Your doctor will use a long, thin (about the width of your little finger), flexible tube with a tiny camera on the end to look inside and through which to pass tools. Endoscopic methods use freezing, electrical or laser heat, or infrared light to wipe out the hemorrhoidal tissue.
A rubber band is put around the base of the hemorrhoid, which cuts off blood flow, and the hemorrhoid withers away within a few days. This technique is used only for internal hemorrhoids.
With this, a chemical is injected around the vein to shrink the hemorrhoid.
Cutting out the hemorrhoids (hemorrhoidectomy) is sometimes suggested but carries a painful recovery.
How to prevent hemorrhoids
Pass your bowel movements as soon as you feel the urge.
Try not to strain to get the stool out.
Be active. Move around, walk and exercise to help move the stools through your body.