What is SIBO?
SIBO stands for small intestinal bacterial overgrowth. This means that you have more than the usual number of bacteria living in your small intestine (bowel).
Certain health conditions can make the intestines more likely to have too many bacteria. These include IBS (irritable bowel syndrome), Crohn’s disease, celiac disease, fatty liver, cirrhosis, short bowel syndrome, pancreatitis, and others.
What are symptoms of SIBO?
There are many common symptoms of SIBO. Eating certain foods may make these symptoms worse.
- Bloating (feeling of being too full that can happen after eating)
- Diarrhea (loose or watery stool 3 or more times a day)
- Constipation (hard-to-pass bowel movements [stool] less than 3 times a week)
- Abdominal or belly pain
- Nausea or upset belly
- Belching or burping
- “Brain fog”
Getting started on nutrition therapy for SIBO
SIBO symptoms are often caused by the gas that is made when extra bacteria use up some types of carbohydrates (sugars and starches found in food that your body uses for energy) in your diet, such as certain types of fiber (a substance in food that helps you pass solid waste), starches and/or sugars. Some people with SIBO find that high fat foods can also make their symptoms worse. Changing your diet can help reduce symptoms of SIBO, but diet alone is not able to cure SIBO.
One popular plan to manage SIBO symptoms is called the low-FODMAP diet. On this diet, patients eat less of certain carbohydrates that are likely to make more gas in the intestines or worsen diarrhea.
FODMAP stands for:
- Fermentable: digestible by bacteria and create gas
- Oligosaccharides: specific types of fiber found in beans, onion, wheat and garlic
- Disaccharide: lactose (or milk sugar) found in milk, yogurt and ice cream
- Monosaccharide: excess fructose, found in honey, mangoes, apples and cherries
- And
- Polyols: natural sugars found in peaches, pears, mushrooms and cauliflower. Sugar substitutes ending in the letters “ol,” like sorbitol and xylitol found in sugar free gums and treats, are also polyols
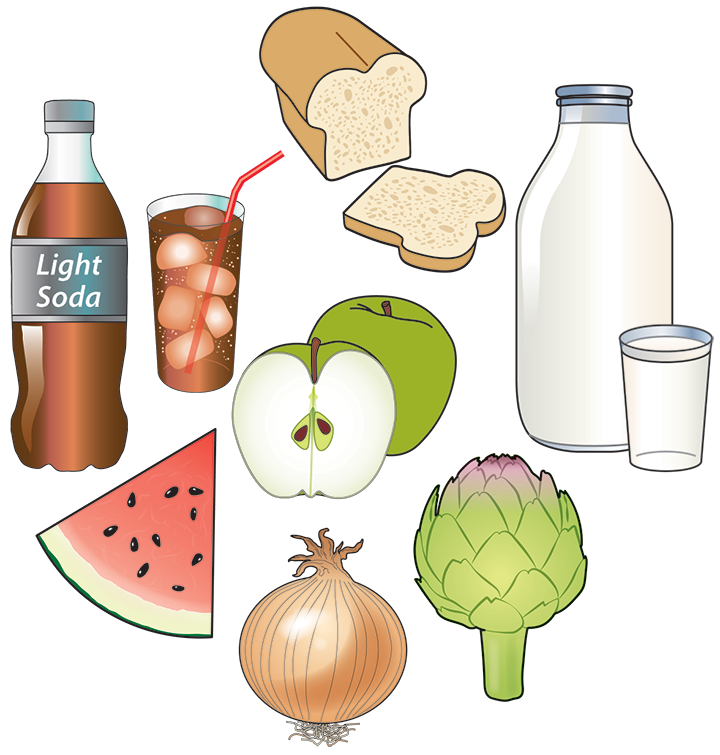
Gluten and dairy are not FODMAPs. A low-FODMAP diet is not gluten-free or dairy-free.
Ideally, a strict low-FODMAP diet should only be followed for as long as you need to follow it to manage your symptoms. Learn more about the low-FODMAP diet and meet with a registered dietitian who can teach you how to get started, and then help you expand your diet when your SIBO is better managed.
Some people with SIBO find that other kinds of carbohydrates or sugary foods can also worsen their symptoms even if they are low-FODMAP. Examples can include rice, cereal, potatoes, large amounts of fruit, table sugar, or desserts. If these types of foods seem to make your symptoms worse, a lower carb diet may be a more helpful approach than a low-FODMAP diet to manage SIBO symptoms.
Meal spacing
Meal spacing helps your body’s natural cleansing waves in the gut. These waves help to keep bacteria levels lower in the small intestine. It is ideal to wait at least 3 hours between meals or snacks, and not to eat too close to bedtime.
Possible nutrient deficiencies
Having SIBO for a long time can block how your body absorbs nutrients. This can lead to weight loss and deficiencies in vitamin B12 and vitamins A, D and E. Talk with your health care provider to check for these possible shortfalls and whether you need to take a dietary supplement.
Resources
Written by
Christine Lothen-Kline, MPH, MCHES, RDN, LDN
Katherine Bennett RD, MPH
Barbara Freedland, MS, RDN
Natalie Rosenbalm (nutrition graduate student)
Reviewed by the DIGID Disorders of the Gut Brain Interaction workgroup, ©2024
Christine Lothen-Kline, MPH, MCHES, RDN, LDN
Katherine Bennett RD, MPH
Barbara Freedland, MS, RDN
Natalie Rosenbalm (nutrition graduate student)
Reviewed by the DIGID Disorders of the Gut Brain Interaction workgroup, ©2024