What are MASLD and MASH?
The liver is one of the most important organs in your body and weighs about three pounds. It sits in the upper-right side of the abdomen (belly), below the ribs.
The functions of your liver include:
- Changing food into energy, metabolizing.
- Helping your body use, medications.
- Removing alcohol and poisons from your system.
- Making bile, which aids in digestion.
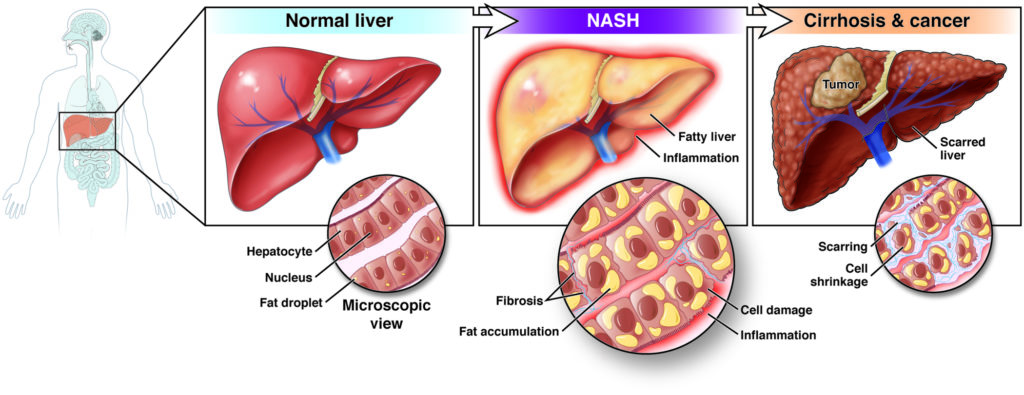
Metabolic dysfunction-associated steatotic liver disease (MASLD) happens when your liver stores too much fat and it is not related to heavy alcohol use.
- MASLD was formerly known as nonalcoholic fatty liver disease (NAFLD).
- MASLD is one of the most common causes of liver disease in the U.S. Between 30-40% of adults in the U.S. have the disorder.
- MASLD is more common in people who have certain conditions, or health problems, such as having obesity and problems that may be related to obesity, like type 2 diabetes.
- People are more likely to develop chronic, or life-long, liver disease as they age. People of any age, including children, can have MASLD.
- MASLD occurs in people of all races and ethnicities.
There are two types of MASLD
Simple fatty liver
When you have fat in your liver but little or no inflammation (swelling) or liver cell damage. Simple fatty liver usually doesn’t cause liver damage or complications.
Metabolic dysfunction-associated steatohepatitis
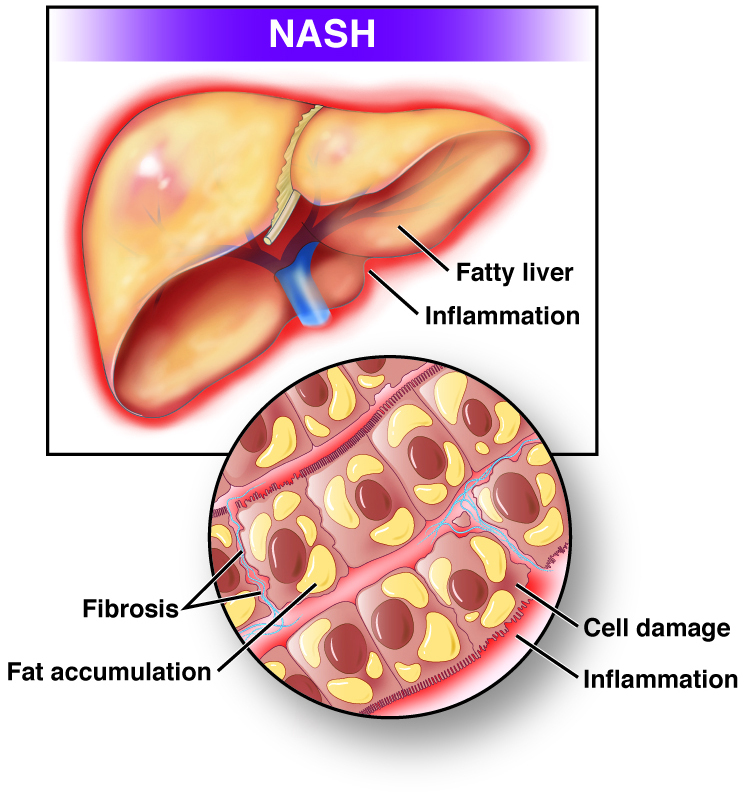
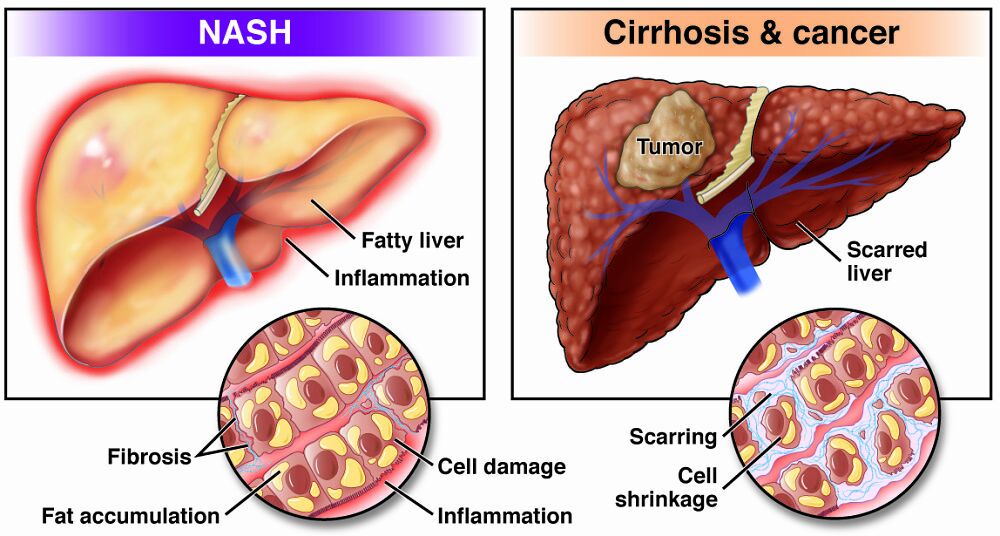
This is a more severe form of nonalcoholic fatty liver disease. In metabolic dysfunction-associated steatohepatitis (MASH; formerly known as nonalcoholic steatohepatitis or NASH), the fat in your liver causes inflammation, called hepatitis, and liver cell damage. In time, this can cause fibrosis, or scarring, of the liver, leading to cirrhosis (permanent scarring or injury to the liver) and liver cancer.
Experts believe that about 20% of people with MASLD also have MASH.
People most often have one type of MASLD, though sometimes, people with one form of MASLD can later be diagnosed with another. Experts are not sure why some people who have MASLD have simple fatty liver while others progress to steatotic liver disease.
Symptoms
Symptoms of MASLD
Fatty liver disease and steatotic liver disease are thought of as “silent diseases,” meaning they have few or no symptoms.
Symptoms of MASH
Even if steatotic liver disease causes you to develop cirrhosis, you still may not have any symptoms.
Possible symptoms include tiredness and pain in the upper-right side of your abdomen (stomach).
Once cirrhosis is advanced, you can develop symptoms such as:
- Swelling in the belly or swelling in the legs.
- Vomiting blood.
- Mental confusion.
A liver transplant may be needed if your liver disease becomes this advanced.
References
Causes
The reasons behind what causes MASLD and MASH are still being studied.
Certain conditions, or health problems, may put you at higher risk for developing MASLD or MASH. Researchers have found that certain genes may make you more likely to develop metabolic dysfunction-associated steatotic liver disease and explain why some MASLD patients have steatotic liver disease while others have simple fatty liver.
Risk factors for MASLD
Being overweight or having obesity, which is having extra body fat over healthy levels or a body mass index (BMI) of 30 or higher.
Having insulin resistance, which is when your body does not use insulin — which controls sugar in your blood — well. This can result in glucose (sugar) in your blood not staying in a normal or healthy range.
Having type 2 diabetes.
Having abnormal levels of fats in your blood:
- High levels of triglycerides.
- High total cholesterol.
- High low-density lipoprotein [LDL] cholesterol, or “bad” cholesterol.
- Low high-density lipoprotein [HDL] cholesterol, or “good” cholesterol.
- Having metabolic syndrome, also called insulin resistance syndrome. This is when you have a large waist size, high blood pressure, or abnormal levels of sugar or fats in your blood.
- Experts think nonalcoholic fatty liver disease may be closely linked to metabolic syndrome.
If you have MASLD, you are more likely to have MASH if you also have one or more of the following:
- Obesity, especially with a large waist size.
- High blood pressure.
- High levels of triglycerides or abnormal levels of cholesterol in your blood.
- Type 2 diabetes.
- Metabolic syndrome.
Less common causes of MASLD and MASH include:
- Health problems that cause your body to use or store fat improperly.
- Rapid weight loss.
- Certain infections, such as hepatitis C.
- Being exposed to some toxins, such as illicit drugs, and workplace chemicals or solvents.
- Medications, such as HIV medications, hormonal medications, seizure medications, arrhythmia medications and supplements. If you do not have other risk factors, such as obesity, diabetes, etc., a medication may be to blame. Your doctor will need to make sure that is not the reason before diagnosing you with nonalcoholic fatty liver disease.
References
Getting Tested for MASLD and MASH
Your gastroenterologist will review your health and medication history, do a physical exam and order certain tests to find out if you have MASLD or MASH.
Your gastroenterologist will ask if you have had certain health conditions:
- Overweight or obesity.
- Insulin resistance.
- High levels of triglycerides or abnormal levels of cholesterol in your blood.
- Metabolic syndrome.
- Type 2 diabetes.
Your doctor will also ask about what kinds of food you eat and lifestyle factors, which can increase your chances of developing MASLD and MASH:
- Lack of physical activity.
- Eating a diet high in sugar and starch.
- Drinking sugary beverages.
Your gastroenterologist may also ask how much alcohol you drink to help decide if alcohol is the cause of fat in your liver and you are showing signs of alcoholic liver disease instead of MASLD.
Your gastroenterologist will check your weight and height to figure out your body mass index (BMI) to confirm if you are underweight, normal weight, overweight or have obesity. He or she will also look for signs of MASLD or MASH:
- An enlarged liver.
- Signs of insulin resistance, like darkened skin patches over your knuckles, elbows and knees.
- Signs of cirrhosis, such as jaundice, which causes the skin and whites of your eyes to turn yellow.
- Signs of advanced cirrhosis — swelling in the legs, fluid in the belly and confusion.
Testing
Your doctor may order blood tests, imaging tests and perhaps a liver biopsy to find out if you have nonalcoholic fatty liver disease or nonalcoholic steatohepatitis.
Blood tests will look for high levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which can mean liver damage.
Imaging tests can help see if you have MASLD:
- Ultrasound uses a device called a transducer to bounce safe, painless sound waves off of your organs to create a picture of their structure.
- Computerized tomography (CT) scans use x-rays and computer technology to create pictures of your liver.
- Magnetic resonance imaging (MRI) machines use radio waves and magnets to make detailed pictures of your organs and soft tissues without using x-rays.
- Transient elastography, otherwise known as Fibroscan, can indirectly measure the amount of fat in the liver and the amount of scarring.
These tests can be performed in an outpatient center or hospital. Ultrasounds are often performed in radiology departments and transient elastography can often be performed in a provider’s office.
These imaging tests can show fat in your liver, but they cannot show swelling of your liver or fibrosis (scarring), or whether you have simple fatty liver or MASH. If you have cirrhosis, the imaging tests may show nodules, or lumps, on your liver.
During a liver biopsy, which can be performed at a hospital or an outpatient center, your gastroenterologist will take a tiny piece of tissue from your liver. You will be told how to get ready for the biopsy beforehand. A pathologist (a doctor who specializes in looking at tissues to diagnose diseases) will then look at the tissue under a microscope to look for signs of damage or disease.
A liver biopsy is the only way to find liver inflammation, or swelling, and damage to diagnose nonalcoholic steatohepatitis. This test is not recommended for everyone with liver disease. A liver biopsy will only be done if you are more likely to have MASH, or if other tests show signs of advanced liver disease or cirrhosis. Sometimes, results of the other testing, such as transient elastography, will help to decide if you are more likely to have MASH and if you would benefit from a liver biopsy.
References
Treatment for steatotic liver disease
Your doctor may recommend weight loss to treat MALFD and MASH. Weight loss can help reduce fat in the liver, inflammation (swelling) and fibrosis (scarring).
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes and being physically active can improve MASLD and MASH. Losing 3-5% of your body weight can lessen the amount of fat in the liver. To reduce liver swelling, you may need to lose up to 10% of your body weight. Doctors recommend slowly losing 7% of your body weight or more over the course of one year. Rapid weight loss through fasting (eating and drinking nothing except water) can make MASLD worse.
Your gastroenterologist may suggest that you meet with a nutritionist or knowledgeable dietitian to talk about and improve your diet. Changing your diet may include eating less fat to help prevent or treat steatotic liver disease. Fats are high in calories and increase your chance of having obesity. Replacing saturated fats and trans fats in your diet with monounsaturated fats and polyunsaturated fats, such as omega-3 fatty acids, may help lessen your chance of heart disease if you have MASLD. Four types of fats are:
- Saturated fats are found in meat, poultry skin, butter, lard, shortening, and all milk and dairy products except fat-free versions.
- Trans fats are found in foods that list hydrogenated or partially hydrogenated oil on the label, such as crackers, snack foods, commercially-baked goods like cookies and cakes, and fried foods.
- Monounsaturated fats are found in olive, peanut and canola oils.
- Polyunsaturated fats are found in greatest amounts in corn, soybean and safflower oils, and many types of nuts. Omega-3 fatty acids are also a type of polyunsaturated fat, which includes oily fish such as salmon, walnuts and flaxseed oil.
Your gastroenterologist or dietitian may also suggest other dietary changes to help treat fatty liver disease and steatotic liver disease:
- Eating more low-glycemic index foods, such as most fruits, vegetables and whole grains.
- These foods affect your blood glucose less than high-glycemic index foods, such as white bread, white rice and potatoes.
- Not consuming foods and drinks that contain large amounts of simple sugars, especially fructose, which is found in sweetened soft drinks, sports drinks, sweetened tea and juices.
- Avoiding alcohol use.
Always speak with your doctor and a nutritionist or knowledgeable dietitian before making changes to your diet, and to help you make a plan you can follow. They may suggest diet plans such as a:
- Low glycemic diet.
- Low carbohydrate (low carb) diet.
- Low carb Mediterranean diet.
- Prediabetes diet.
- Plant-forward diet.
If you have severe obesity —a body mass index (BMI) of 35 to 40 or more — and have not been able to lose or maintain weight loss, your gastroenterologist may suggest bariatric surgery, an operation that helps you lose weight by making changes to your digestive system. Bariatric surgery may also be an option if you have serious health problems, such as type 2 diabetes or sleep apnea, related to having obesity. Learn more about bariatric surgery and other weight loss treatments on our patient education page about obesity.
Currently, there are no drugs that have been approved to treat MSALD or MASH, but researchers are studying medicines that may improve these conditions.
While some studies have shown that supplements may help improve MASLD or MASH, for safety reasons, always speak with your health care provider before using dietary supplements, such as vitamins, or any complementary or alternative medicines or medical practices. Some herbal remedies can cause more damage your liver.
Clinical trials
Researchers are studying many aspects of MASLD and MASH through clinical trials, which include:
- Building databases of adults and children who have MASLD.
- Comparing how people with and without MASLD process and metabolize food.
- Studying how weight-loss surgery affects MASLD in adolescents.
- Evaluating new medicines/new treatment for MASH.
You can view a filtered list of clinical studies on NAFLD and NASH that are federally funded, open and recruiting at www.ClinicalTrials.gov. Always talk with your health care provider first before participating in a clinical study.
Support groups
Support groups are available to help you through your diagnosis. Learn more at the American Liver Foundation website.
Complications of MASLD and MASH
Most people with MASLD have simple fatty liver and people with simple fatty liver typically don’t develop complications. However, people with MASH have an increased chance of dying from liver-related causes. For example, if cirrhosis develops and progresses to liver failure, you may need a liver transplant. Studies also suggest that people with MASLD have a greater chance of developing cardiovascular disease, which is the most common cause of death in people who have either form of MASLD.
It is important to work with your doctor and other health care providers to monitor your condition and make any needed modifications to your diet or daily habits, as well as follow any recommendations to gradually lose weight if you are overweight or have obesity. You may be able to prevent MASLD and MASH by eating a healthy diet, limiting your portion sizes and maintaining a healthy weight.