What is diverticulitis?
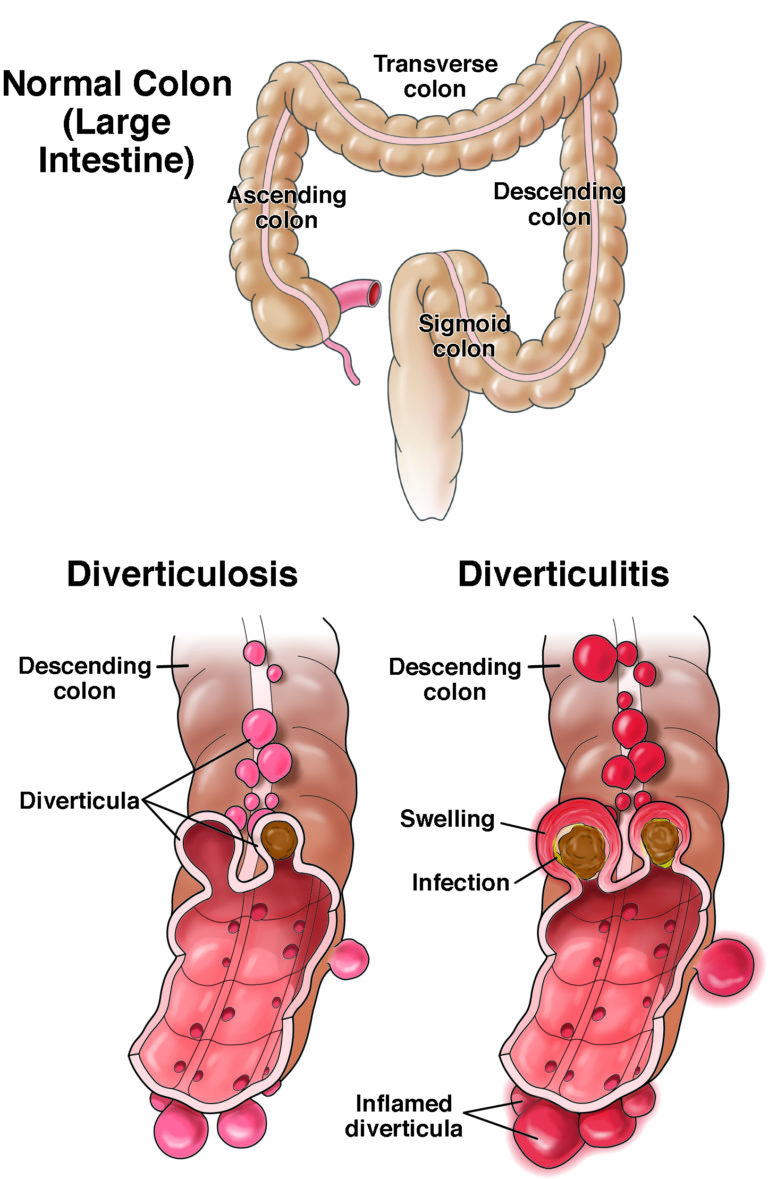
By age 50, about half of people have diverticulosis, a health issue in which pockets (or diverticula) form in the wall of the large bowel. In about 5% of people, these pockets may become acutely inflamed, or swollen, which is called diverticulitis.
Diverticulitis can be painful. It often comes about quickly
Diverticulitis may need to be treated with an antibiotic.
Recent data reveals that 20% of people with diverticulitis have recurrent flare-ups, often within five years of the first attack. There are steps you can take to lower the risk of future attacks.
In Western countries, diverticulitis is most common in women over the age of 60. Based on limited evidence, diverticulitis is more common in non-Hispanic Whites compared with other races.
What are the symptoms of diverticulitis?
Symptoms of diverticulitis include:
- Abdominal, or belly, pain and cramping, soreness, often on the lower left side.
- Fever.
- A change in bowel habits, such as diarrhea (loose stool) or constipation (hard stool or trouble passing stool).
- Nausea.
- Throwing up.
- Chills.
Who’s at risk for diverticulitis?
Diverticulitis can often be suspected based on your past health issues and a physical exam, though other tests may be needed, as well. Your doctor will talk to you about what is best for you.
Tests for diverticulitis
CT scan
This is the most common test to find diverticulitis. You will either drink a special liquid and/or have the liquid put into your vein, which will help light your organs on an X-ray so that your doctor is able to see them better.
Other tests
- Blood test: You may have blood drawn for further evaluation.
- Stool sample: You may submit your stool to be looked at under a microscope.
Treatment for diverticulitis
Uncomplicated diverticulitis is treated with plenty of rest and possibly antibiotics.
Some people with more severe or complicated diverticulitis may be admitted to the hospital for intravenous antibiotics, drainage of abscesses or emergency surgery.
Once treated, most people start feeling better within days to a few weeks. If your diverticulitis keeps coming back, you may think about having surgery to remove a part of your colon.
Ways to try to stop diverticulitis from coming back
After your diverticulitis is cleared, slowly start adding more fiber to your diet. Try eating at least eight grams of fiber in each meal. Good foods to have in your meals to get more fiber include, berries, beans, green veggies, grains/oats. Note: You do not have to avoid seeds, nuts or popcorn.
Working out for 30 minutes five times a week could help stop future attacks. Your workout should get your heart pumping and make you start to sweat. Good workouts include: jogging, swimming, aerobics classes and competitive sports.
Questions to ask your doctor
1. How can I tell if I am getting enough fiber in my daily diet?
2. Am I healthy enough to start (or carry on with) working out after I get better?
3. Should I avoid aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen)? These may increase your risk of diverticulitis.
4. Should I get a colonoscopy?
Complications of diverticulitis
Issues that could come from diverticulitis include:
- A block in the colon.
- An infection.
- A tear (perforation) in the colon.
- An abscess (sore).
- Urinary tract infections.
In rare cases, diverticulitis can be a warning sign for colon cancer. Getting a colonoscopy can rule this out. If you have not had a colonoscopy lately, talk to your doctor about getting one a couple months after you feel better.
Reviewed by

Anne Peery
MD
Assistant professor, University of North Carolina, Chapel Hill

Anne Peery
MD
Assistant professor, University of North Carolina, Chapel Hill