What is Crohn’s disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD).
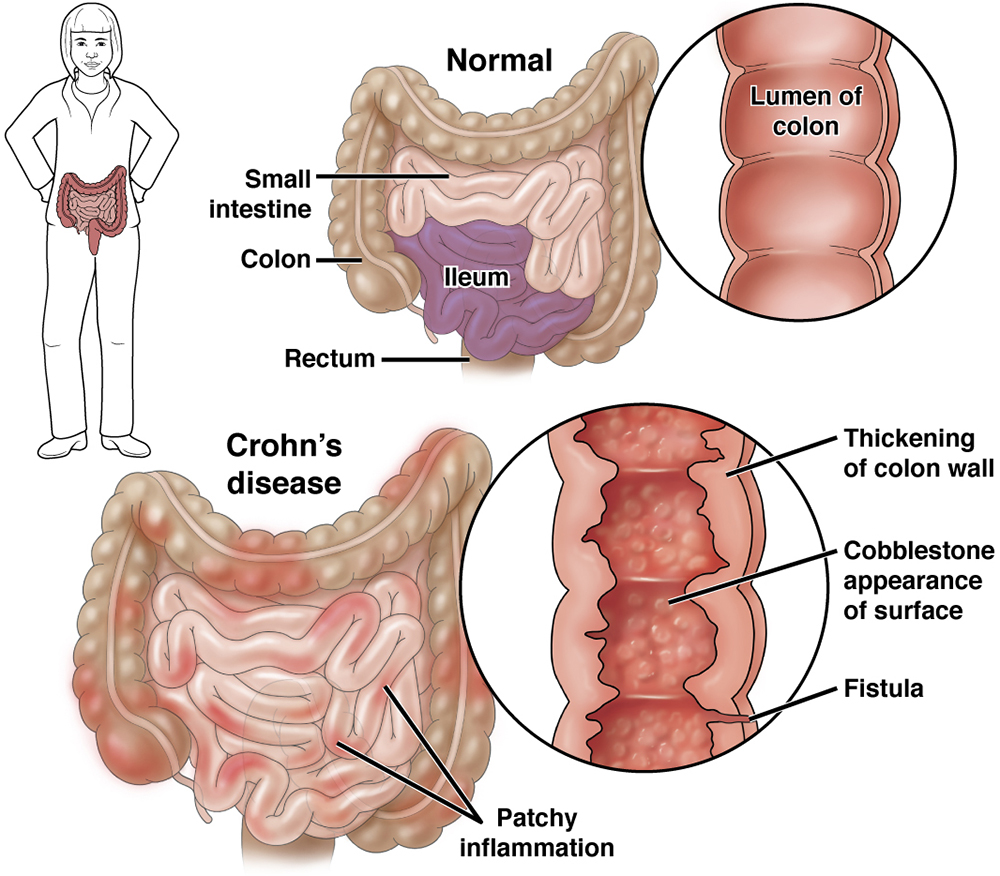
Crohn’s disease causes inflammation (pain and swelling) in the gastrointestinal (GI) tract, also called the digestive system. Inflammation from Crohn’s disease can make it hard for you to take in nutrients during digestion. Crohn’s disease can have times of remission (time when you feel well) and relapse (when you feel ill).
While there is no cure for Crohn’s disease, there are treatments that can help.
The most common part of the body affected is the lower part of the small intestine, called the ileum, and the first part of the colon. However, Crohn’s disease can show up in any part of the GI tract, from the mouth to the anus.
Who gets Crohn’s disease?
Crohn’s disease can be found in people of any age but is often found between ages 13 and 30. Crohn’s disease can occur in people of all races and ethnicities and is increasing all over the world. The extension of the disease has been reported to be greater in African Americans, Hispanics and Asians.
What causes Crohn’s disease?
Right now, the cause of Crohn’s disease is not fully known. Experts think a few things could play a role in getting Crohn’s disease:
Crohn’s disease is thought to be an autoimmune health issue, meaning the body’s immune system thinks food and other things are not supposed to be there. With this, the body attacks your gut, causing inflammation.
Crohn’s disease tends to run in families. Different variants of specific genes have been associated with Crohn’s disease in Asian, Black and White patients.
Some studies show certain things, such as the use of nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, oral contraceptives or a high-fat diet may slightly raise chances of getting Crohn’s disease. Smoking can raise the chances of getting Crohn’s disease.
Stress or certain foods do not cause Crohn’s disease. However, high stress and some foods may worsen symptoms.
Newly diagnosed with Crohn’s disease
No matter what you may be feeling upon hearing you have Crohn’s disease, it is of great value to know that you are not alone and that many places have support groups, both in-person and online, for people all ages with Crohn’s disease that can be very helpful.
If you are overwhelmed by your new diagnosis, don’t wait to reach out to a mental health expert to talk through the changes. Relaxation techniques, such as yoga, meditation or mindfulness, may be very helpful.
Working together with your health-care team, you can make a treatment plan just for you, to help control your symptoms and put you in charge of your Crohn’s disease.
Questions to ask your doctor
1. How often do I need to see a gastroenterologist?
2. How often do I need to undergo testing?
3. What are my risks for colon cancer?
4. Are there symptoms that should cause worry? If so, what are they?
5. If you don’t know something at any point, ask for more (or clearer) information! For some, hearing that they have Crohn’s disease is a relief, a reason for symptoms and a light at the end of the tunnel. For others, it can be scary and daunting. Many will have a mix of feelings. All of this is completely normal.
- How often do I need to see a gastroenterologist?
- How often do I need to undergo testing?
- What are my risks for colon cancer?
- Are there symptoms that should cause worry? If so, what are they?
- If you don’t know something at any point, ask for more (or clearer) information! For some, hearing that they have Crohn’s disease is a relief, a reason for symptoms and a light at the end of the tunnel. For others, it can be scary and daunting. Many will have a mix of feelings. All of this is completely normal.
What are the symptoms of Crohn’s disease
The symptoms of Crohn’s disease can vary from person to person, based on where the disease is in the body and how bad the inflammation is.
The most common symptoms of Crohn’s disease are:
- Belly pain and cramps, often in the lower right side.
- Diarrhea (loose stool).
- Weight loss.
- Rectal bleeding.
- Fever.
- Feeling tired or weak.
- Loss of appetite.
- Anemia (low iron in your blood, which can make you feel weak and tired).
- Joint pain.
- Changes in skin (red bumps that are tender when touched).
- Eye irritation.
- Delayed development and stunted growth in children who have the disease.
Tests for Crohn’s disease
The diagnosis of Crohn’s disease will usually require an evaluation by a gastroenterologist.
Depending on your health insurance, this may require a referral from your primary care physician and authorization from your medical insurer. This may also be a requirement for some of the special tests that the gastroenterologist will order to confirm the diagnosis and establish treatment.
There are many tests your gastroenterologist can do to find out if you have Crohn’s disease.
First, he or she will take your past health info, listen to your symptoms, and do an exam to feel and listen to your belly. No one test makes the diagnosis, but testing is used to confirm the gastroenterologist’s clinical suspicion that Crohn’s disease is causing symptoms.
Talk to your doctor about which test is best for you. Your doctor will give you specific instructions for how to get ready for your test for Crohn’s disease.
Blood tests
- Your doctor will look for anemia (low iron in your blood, which can make you feel weak and tired), caused by bleeding.
- Blood tests can show signs of inflammation or infection somewhere in the body, like a high white blood cell count and other markers of inflammation.
- Blood tests can be done at your doctor’s office or in a lab.
Stool tests
- Stool tests are done to make sure there aren’t other GI health problems, such as infection, causing symptoms.
- Stool tests can show if there is bleeding in the intestines and may confirm if inflammation is present.
- Your doctor will give you a special holder for the stool, which is then returned to your doctor or a lab.
Procedures
The below tests are done in your doctor’s office, an outpatient center or a hospital. These tests can be used to find Crohn’s disease or to rule out other health issues, such as ulcerative colitis, irritable bowel syndrome (IBS), diverticulitis or cancer.
- A colonoscopy involves looking at the colon from inside the body using a long, thin (about the width of your little finger), flexible tube with a tiny camera on the end, through which the doctor can view your whole colon and rectum for inflammation, swollen tissue, ulcers or polyps (mushroom-like or flat growths on the inside wall of the colon or rectum).
- If the doctor thinks it might be Crohn’s disease, he or she will also do a biopsy (taking a small piece of tissue to look at under the microscope) during the colonoscopy. This is not something you will be able to feel.
- You might feel some pressure during the exam and there may be some cramping afterward, but you most likely will not feel a thing during this test.
- You will need to “prep” before this test to clean out your bowel so your doctor can see clearly. Follow the instructions given to you by your doctor to do this.
- Since you will be given medicine to make you sleepy, you will need someone to take you home and you won’t be able to go to work that day. The next day, most people go back their usual activities.
- An endoscopy or enteroscopy is done to look inside your gastrointestinal (GI) tract to see if there is inflammation or ulcers and to get a small piece of the tissue (biopsy) from your small intestine to see if Crohn’s disease is present.
- You will be given medicine to block pain and make you feel relaxed and sleepy, so you won’t feel much during the test.
- During the endoscopy, your gastroenterologist will use a long, thin (about the width of your little finger), flexible tube with a tiny camera on the end to look inside.
- The tube is passed through the mouth into the small intestine as your gastroenterologist does a careful exam.
- A capsule endoscopy is a way for your doctor to see inside your GI tract and look at the lining of the small intestine.
- Unlike an upper GI endoscopy or a colonoscopy, this test uses a camera inside a pill-like capsule.
- You will swallow the pill (which is just over 1-inch long and less than ½-inch wide) at your doctor’s office.
- Once swallowed, it will travel through your GI tract, sending images to a special device for your doctor to review.
- You will be awake and active during this test, though you will not feel the capsule. The capsule will leave your body naturally through a bowel movement.
- These tests use both X-rays and computer technology to make clear images for your doctor to see your GI tract.
- You will need to drink a mixture, which helps your doctor see your GI tract more clearly on the images. You may also be injected with a dye to help, as well.
- You will not be put to sleep for this test.
- This test can find Crohn’s disease and complications from the disease.
- This test uses X-rays to look at your upper GI tract.
- During this test, you will sit or stand in front of an X-ray machine and drink a thick liquid called barium. The barium will coat your esophagus (the tube that links your mouth and stomach), stomach and small intestine so your doctor can see them more clearly in the images.
- You will not be put to sleep for this test.
- You should not eat or drink before this test.
- This test may cause bloating (swelling) or upset belly for a short time. The barium may cause your stool to be white or light-colored. You may be instructed to take a laxative after the test to make sure that the barium is passed and does not cause severe constipation (hard stool or trouble passing stool).
How is Crohn’s disease treated?
While there is no cure for Crohn’s disease, there are a number of options to help treat it. The goals of treatment are to:
- Control inflammation, or swelling.
- Ease symptoms, like pain, diarrhea (loose stool) and bleeding.
- Fix nutrition deficiencies, if needed.
Treatment will depend on where the disease is and the severity of the disease, past complications, and response to earlier treatments. Remember, everyone experiences symptoms of Crohn’s disease differently. If one treatment doesn’t work as well, there are other options. Just be sure to be in touch with your doctor regularly. Treatment options for Crohn’s disease involve medications, nutrition supplementation, surgery or a combination.
Medications
The goals of using medications are to start or keep up remission (no symptoms) and to improve quality of life. Each person reacts a little bit differently to each drug and many need a combination of drugs. While some of them have side effects, the benefits and symptom relief often outweigh those drawbacks.
Access to medications may be determined by your health insurance coverage. Some medications may not be covered by your insurance, or your insurer may require that other drugs be used first before “stepping up” therapy. Insurers may also require the use of bioequivalent drugs or biosimilar agents when these are available. Your gastroenterologist may help you in getting approval of this medications. Patient assistance programs from pharmaceutical companies or foundations may be of help in getting access to the prescribed medications.
Aminosalicylates help control inflammation, especially in those who are newly diagnosed with mild symptoms. Sometimes these drugs are called 5-ASA’s, which stands for 5-aminosalyciclic acid.
- Examples include:
- Balsalazide.
- Mesalamine.
- Olsalazine.
- Sulfasalazine.
- Possible side effects:
- Belly pain.
- Diarrhea (loose stool).
- Headaches.
- Heartburn.
- Nausea and throwing up.
Corticosteroids can be very helpful right away. They help lessen inflammation quickly. These drugs are often given in large doses when the disease is at its worst, then lowered as symptoms get under control. They are given to people with moderate to severe symptoms and are not given for long-term use.
Examples include:
- Prednisone.
- Budesonide.
- Hydrocortisone.
- Methylprednisolone.
Possible side effects include:
- Weight gain.
- Acne.
- Facial hair.
- Mood swings.
- Bone mass loss.
- Greater risk of infection.
- Hypertension.
- High blood sugar (diabetes).
Stopping these drugs suddenly could cause withdrawal symptoms, so your doctor will have you lower the dose slowly.
Immunomodulators, or immunosuppressive agents, block the immune reaction that leads to inflammation, lessening inflammation in the gastrointestinal (GI) tract. These drugs can take up to three months to start working, so they are often used with other medicines until that time. Immunomodulators are given to help people go into remission or given to people who have not responded to other treatments.
Examples include:
- 6-mercaptopurine (6-MP).
- Methotrexate.
- Azathioprine.
Possible side effects include:
- Nausea or throwing up.
- Diarrhea (loose stool).
- Less able to fight infections (from low white blood cell count).
- Fatigue or feeling tired.
- Pancreatitis.
Biologic treatments drugs can lessen inflammation and quickly bring on remission of Crohn’s disease. These drugs are used in people with moderate to severe Crohn’s disease who do not respond to other treatments.
Biologics are often given by either injection or infusion every six to eight weeks, based on what the patient needs. These drugs tend to cost more, so talk to your health plan before starting.
Examples include (brand names may be different):
- Infliximab.
- Adalimumab.
- Certolizumab.
- Vedolizumab.
- Natalizumab.
- Ustekinumab.
Possible side effects include:
- Toxic/allergic reaction.
- Itching or bruising at injection or infusion site.
- Greater chance of getting infections (especially tuberculosis).*
- Greater chance of lymphoma.*
*Less chance of infection or lymphoma with Vedolizumab.
There is a new type of biologic treatment, known as biosimilar products. Biosimilars have been approved by the U.S. Food and Drug Administration (FDA) to use as treatment in place of existing biologic drugs. They are highly similar to originator biologic drugs and have no clinically meaningful differences, though they are not generic drugs.
Your doctor can prescribe a biosimilar as a substitute for a biologic drug; however, your pharmacist cannot change you from a biologic drug to a biosimilar without your doctor’s approval.
Overall, biosimilar products should produce the same effects as a standard biologic drug. Talk to your doctor about more information and what is best for you to treat your Crohn’s disease.
Examples include:
- Infliximab-dyyb (Inflectra).
- Infliximab-abda (Renflexis).
- Infliximab-axxq (Avsola).
Possible side effects are the same as those for biologic drugs.
OTHER MEDICATIONS
Acetaminophen can be used for mild pain.
People with Crohn’s disease should not take ibuprofen, aspirin or naproxen as they can make symptoms worse or cause GI bleeding.
- Antibiotics are given to prevent or treat infections and fistulas (a link between two body parts that should not be there, such as between two organs; they can form from infection, inflammation or surgery).
- Loperamide is given to help slow or stop severe diarrhea. It should only be taken for short cycles of time.
Nutrition supplementation
Some nutrition options for people with Crohn’s disease are:
- Staying away from carbonated drinks.
- Avoiding popcorn, raw veggies, nuts and other high-fiber foods.
- Drinking more liquids (not alcohol). Oral rehydration solution (such as Pedialyte®) is good.
- Eating smaller meals more often.
- Keeping a food journal to track symptoms.
- Using a nutrition supplement or vitamin.
Bowel rest
Surgery for Crohn’s disease
Medication helps many patients with Crohn’s disease, but for some, it is not enough to help relieve symptoms. Up to 85 percent of patients with Crohn’s disease will need surgery at some point. Surgery is not a cure, though it can help ease symptoms or treat any complications.
Surgery is often a last resort and used when a patient has:
-
Bowel blockage.
-
Bleeding that won’t stop.
-
Fistulas.
-
Abscess.
-
Symptoms that don’t get better with medication.
Types of surgery for Crohn’s disease
There are a few types of surgery that can be done for Crohn’s disease. A surgeon will work with you and your gastroenterologist to figure out if you need surgery and which surgery would be best. For any surgery, you will get general anesthesia (be put totally to sleep) and will be in the hospital for up to a week after. It can take up to six weeks for patients to fully heal after surgery.
This surgery is done to remove part of the small bowel. It is done when there is a block or severe disease in the small bowel that does not get better with medicine.
The surgeon will take out the part of the bowel and reconnect the healthy ends of the bowel.
This surgery can be done laparoscopically or as an open surgery.
- Laparoscopic — Uses a few small, ½-inch incisions in the belly to put in a thin tube with a camera on the end. Looking at the images from the camera, the surgeon put tools through the small incisions to complete the surgery.
- Open — Uses one 6-inch incision in the belly.
This surgery is sometimes called a large bowel resection, meaning it removes part of the large bowel. It is done when there is a block, a fistula or severe disease in the large bowel that does not get better from medicine. The surgeon will take out the part of the bowel and reconnect the healthy ends of the bowel.
This surgery can be done laparoscopically or as an open surgery.
- Laparoscopic — Uses a few small, ½-inch incisions in the belly to put in a thin tube with a camera on the end. Looking at the images from the camera, the surgeon puts tools through the small incisions to complete the surgery.
- Open — Uses one 6-inch incision in the belly.
This surgery is done to take out the whole large bowel and rectum.
An ileostomy is a small hole in the belly. The last part of the small bowel, the ileum, ends at this hole outside of the body. A removable, external pouch (ostomy pouch) is connected to the hole to collect the content of your intestines (stool). The ileostomy may be temporary or permanent.
With total removal of the colon and rectum (proctocolectomy), you will have the ostomy for the rest of your life.
Complications
Taking your medicine and staying well hydrated and nourished can help keep Crohn’s disease under control. Sometimes, though, complications can happen. Often, with Crohn’s disease, these issues will need medical attention. If you think you are having one of these complications of Crohn’s disease, let your doctor know right away.
A block or a stricture (when the bowel is very narrow in one spot) can happen. Crohn’s disease can thicken the bowel wall with swelling or scar tissue, causing the block or stricture. A block can stop food or stool from passing through the bowel as it is supposed to. A block can sometimes be treated with medicine, but often needs surgery.
A fistula is a link (or tunnel) between two body parts that should not be there, such as between two organs. They can form from infection, inflammation or surgery. Fistulas often form near the anus and rectum in patients with Crohn’s disease.
Fistulas can heal with medicine or changes in diet, but some may need surgery.
Perianal disease (perianal ulcers, fissures and fistulas) has been reported more frequently in Blacks, South Asians and Hispanics.
If Crohn’s disease is not under control, it can stop the body from getting the vitamins, minerals and nutrients it needs. This can be treated with IV fluids or feeding tubes to help patients get the nutrition they need while they work with their doctors to get the disease under control.
Inflammation from Crohn’s disease is often found in the bowel or along the gastrointestinal (GI) tract, but sometimes the immune system causes inflammation in other places like the joints, eyes and skin. Medicines to help with pain and to help get inflammation under control are used to treat this.
Ulcers are open sores. Ulcers can form from inflammation anywhere on the GI tract, the mouth, bowels, anus or perineum (place between the anus and the sex organs). Medicines for Crohn’s disease often treat ulcers, as well.
Perianal disease (perianal ulcers, fissures and fistulas) has been reported more frequently in Blacks, South Asians and Hispanics.
Anal fissures are small tears or cuts found in the anus. They may cause itching, pain or bleeding. Often, fissures get better with medicine, ointments, warm baths and changes in diet.
Perianal disease (perianal ulcers, fissures and fistulas) has been reported more frequently in Blacks, South Asians and Hispanics.
Reviewed by

Esther A. Torres
MD, AGAF
professor of medicine, University of Puerto Rico School of Medicine, San Juan

Esther A. Torres
MD, AGAF
professor of medicine, University of Puerto Rico School of Medicine, San Juan