Overview
Under the Affordable Care Act, certain preventive health care tests, which can help find or prevent serious diseases or health problems, are free to patients, including colorectal cancer screening. Colonoscopy is one of these tests and while it is often free, there are some times when a coinsurance payment is required.
The good news — new policies are making colorectal cancer screening free to more people and getting rid of surprise bills.
Read this guide to learn what to expect and what to do if you get a bill you were not expecting after having a colorectal cancer screening.
You can now get screened for colorectal cancer beginning at age 45.
Here are the most common screening tests, how often they’re needed, and what you can usually expect to pay depending on whether you have commercial (private) health insurance or Medicare (government health insurance program; coverage may be dependent on whether you have original Medicare or Medicare Advantage).
Read more about each colorectal cancer screening test.
- Non-invasive test for people at average risk for colon cancer [no family history, gastrointestinal (GI) symptoms or inflammatory bowel disease (IBD), including Crohn’s disease or ulcerative colitis], like fecal immunochemical testing (FIT) or a multi-targeted stool DNA test (like Cologuard®).*
- Done every 1-3 years (depending on the type of test) starting at age 45 to look for DNA changes and small amounts of blood in the stool that could come from colon cancer or pre-cancerous polyps. A colonoscopy is needed if the stool test is positive.
- Commercial insurance: Pays for both the stool-based test and colonoscopy (including polyp removal) after a positive stool test if it was done after May 31, 2022. For tests performed before May 31, 2022, the stool-based test is covered at 100%, but you might have to pay some of the costs for the colonoscopy.
- Medicare: Pays for both the stool-based test and colonoscopy at no cost, but you may have to pay some of the cost of the colonoscopy if you have polyp(s) removed.
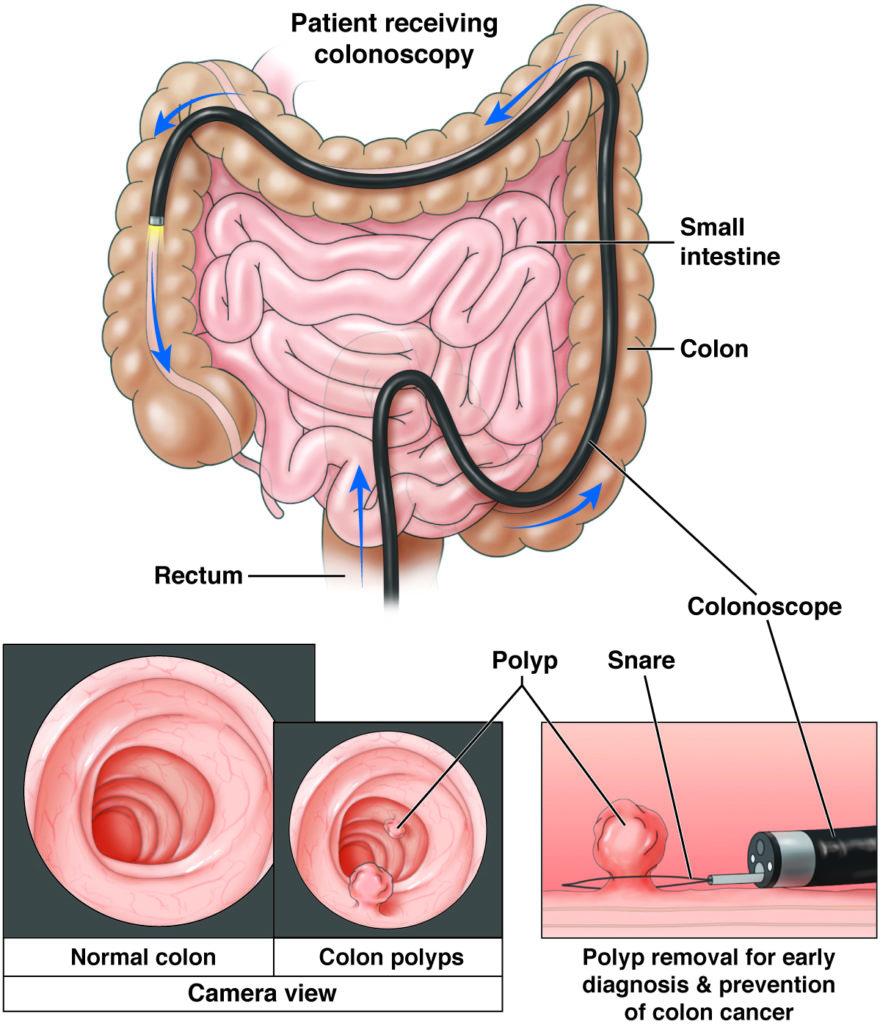
- Procedure for people at average risk for colon cancer.
- Done every 10 years starting at age 45 to look for (and remove, if needed) colon polyps in patients who do not have any symptoms, such as bleeding, gut pain or diarrhea.
- Commercial insurance: Costs for your colonoscopy, bowel prep, sedation (medicine to put you to sleep), lab work, and the hospital or ambulatory surgery center where the colonoscopy was done are covered 100% by health insurance even if polyps are removed.
- Medicare: Colonoscopy and sedation are covered 100% when no polyps are found. In 2022, if a polyp is taken out you are responsible for 20% of the cost. From 2023 to 2026, your responsibility is 15% of the cost, from 2027 to 2029 it falls to 10%, and by 2030 it will be covered 100% by Medicare.
- Procedure for people at higher risk for colon cancer or with certain GI symptoms.
- Done to look for inflammation, or swelling, in patients who have IBD, bleeding, or other GI symptoms, such as rectal bleeding or blood in the stool (bright red, black or very dark), gut pain, or diarrhea.
- Not fully covered by Medicare or commercial insurance, meaning you may have to pay some of the costs, including those for the bowel prep, sedation, lab work, and the hospital or ambulatory surgery center costs where the colonoscopy was done.
Unexpected colonoscopy bill
Contact your gastroenterologist’s office.
- Patients with commercial (private) health insurance: Ask if they used modifier 33 with the colonoscopy. If not, ask them to resubmit the claim.
- Patients with Medicare: Ask if they used modifier KX with the colonoscopy. If not, ask them to resubmit the claim.
Contact your insurance.
- Tell them the U.S. Department of Labor (DOL) put out new guidance that health plans and insurers “must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive non-invasive stool-based screening test” for plan or policy years beginning on or after May 31, 2022.
- See Coverage of Colonoscopies Pursuant to USPSTF Recommendations (page 11) and questions 7 (page 12) and 8 (page 12) of the DOL FAQ About Affordable Care Act Implementation.
Contact your insurance company.
- Tell them the U.S. Department of Health and Human Services (HHS) put out guidance that “the plan or issuer may not impose cost-sharing with respect to a polyp removal during a colonoscopy performed as a screening procedure.”
- See question 5 of the HHS Affordable Care Act Implementation FAQs.
What to do if your insurance company still won't pay
-
Find out when your plan was created
If your plan was created on or before March 23, 2010, or if you have an employer-sponsored health care plan, it does not need to offer all the benefits and protections of the Affordable Care Act nor does it need to cover colonoscopy after a positive stool-based test.
-
Ask why the colonoscopy claim was denied
If the insurer says the medical coding was incorrect, call your gastroenterology practice and ask for help to work with the insurance company.
-
Use social media
Tag your insurer and ask why they won’t pay for your colonoscopy as part of their colorectal cancer screening benefit.
-
File a complaint
File a complaint with the State Insurance Commissioner or at the federal level if your state doesn’t have an external review process.
* Reference to any specific product, service, process, or method by trade name, trademark, service mark, manufacturer or otherwise does not constitute an implied or expressed recommendation or endorsement by AGA.
Updated: Feb. 21, 2023