Welcome to the Obesity Resource Center
If you or someone you care about is struggling to maintain a healthy weight, you’re not alone. Most American adults are overweight or obese. The good news? There are many ways to manage your weight, and you’ll find helpful information and resources about them here.
Overview
What is obesity?
Obesity is a medical condition in which too much body fat negatively impacts your health. It is healthy to have some body fat. In fact, a healthy level of body fat is needed to survive. But too much fat can be harmful to your body.
Obesity is most often measured by Body Mass Index (BMI), a calculation of body weight compared with height. BMI isn’t the only way to measure healthy weight. There are other factors involved (like muscle mass), but national guidelines define obesity based on BMI:
- Someone is a healthy weight if their BMI is 18.5–24.9.
- Someone is overweight if their BMI is 25.0–29.9.
- Someone has obesity if their BMI is 30 or higher.
To figure out your BMI, use this online calculator.
How does obesity impact health?
Obesity can have many harmful health effects. It impacts your body because of the way fat cells act. For instance, having excess fat cells can cause low-level inflammation (swelling) throughout your body. This can harm your blood vessels, muscles (including the heart), and organs (like the liver and pancreas). Inflammation can raise your risk for many types of cancer. It can also cause joint and muscle pain as well as breathing problems at night (called obstructive sleep apnea).
Studies have shown a link between obesity and a higher risk of many health issues, including:
- Heart disease
- Stroke
- Type 2 diabetes
- Metabolic dysfunction-associated steatotic liver disease (MASLD)
- Gastroesophageal reflux disease (GERD)
- Certain types of cancer (like endometrial, breast and colon cancer)
- Infertility
- Osteoarthritis
- Depression
- Sleep apnea
- Chronic pain
- High blood pressure
- High cholesterol
- High triglycerides
What causes obesity?
There are many things that can raise a person’s risk of obesity:
Modern life (with cars, working from home and digital devices) has made people less physically active.
For instance, many people turn to food when they’re depressed or stressed.
Excess weight can come from other health issues or treatment of those health issues. For instance, low thyroid hormones can slow metabolism and cause weight gain. Some medications can cause weight gain too.
Obesity can run in families, so a person whose parent or grandparent has obesity may be at higher risk.
- There was a time when humans had to hunt or gather their own food. So, our bodies stored calories to keep from starving when there was little food. Even though food is easier to get now, our bodies haven’t fully adapted.
- Also, special hormones and other substances in the body can impact feelings of hunger and fullness. Some people with obesity may not feel full as a result.
- Lack of sleep can also be a factor in weight gain.
But there are many things you can do to help prevent or treat obesity. If you’re looking for help, you’re not alone and you’re in the right place.
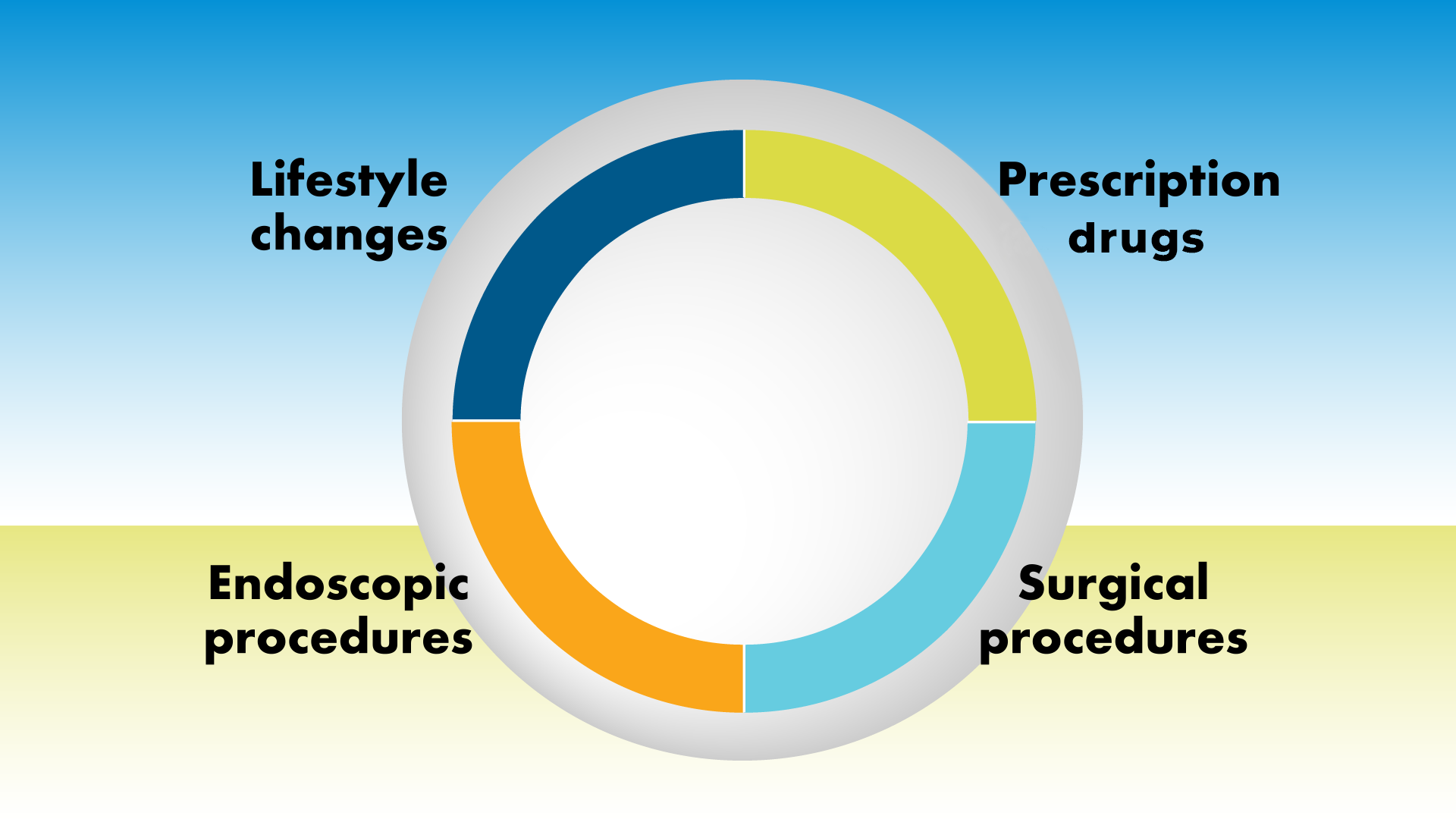
Treatment options
Lifestyle changes to manage weight — and overall wellness — include healthy eating and regular physical activity. No matter what other approach(es) your health care provider might suggest, healthy eating and physical activity are usually also recommended. Try these healthy lifestyle changes on your own, with family or friends, or as part of a weight loss program.
If lifestyle changes alone have not been enough to help you manage weight, your health care provider may suggest a prescription drug. Most medications work by lowering your appetite, so you eat less. Talk to your provider about which drug is right for you because many have side effects or can’t be taken with other medications. You should also ask about over-the-counter medications before trying any.
Endoscopic procedures fill or change the shape of the stomach temporarily to make you feel full faster and “jump start” weight loss efforts.
Obesity surgeries (like laparoscopic sleeve gastrectomy, laparoscopic Roux-en-Y gastric bypass or modified duodenal switch) are major surgeries that seal off large portions of the stomach. These surgeries call for ongoing lifestyle changes and monitoring by your health care team.
Decision tool
How to talk with your health care provider about weight loss and treatment options:
If you think your weight may be impacting your health, it’s important to talk with your health care provider about your concerns and what your options are. It can be a hard topic to bring up, but open communication with your provider is a key step in being healthy.
Don’t wait for your health care provider to bring it up. Use this tool to get the conversation started. When your provider understands your health, personal history and goals, you can work together to find the option(s) right for you.
Consider asking these questions to start the conversation.
- Does my current weight put me at risk for health issues?
- What health issues am I at risk for?
- How would you recommend I try to manage my weight?
- What should my weight loss goal be?
- What are the next steps for me?
Describe your health concerns, including any conditions you may have.
- Tell your provider about any conditions you have. They may be related to weight or inform what weight loss options might be best for you.
- Remind them of any medications you are currently taking.
Explain where you are on your weight loss journey.
- Tell your provider about your history, including how long you’ve been at your current weight, and whether you’ve gained or lost weight throughout your life.
- Outline any past efforts to lose weight and what approaches you’ve tried. Consider filling out this chart before your visit and bringing it with you.
- Tell them how you’re feeling about your weight. This can be hard, but it’s important for them to understand what you’re experiencing.
- Talk about your health goals and hopes for the future.
Ask what option(s) might be right for you.
Here are factors your health care provider will likely want to discuss and consider before making any recommendations:
- Your overall health and any conditions you have.
- Your past efforts to lose weight.
- Your health goals.
- Your Body Mass Index (BMI). This is a calcuation based on your height and weight. It’s one of the main ways health care providers think about weight and what options are right for different people.
Once your health care provider understands your health history, profile and goals, together you can discuss the weight loss options that might be right for you. They might include one or more of the following approaches.
Lifestyle changes
Healthy eating and regular physical activity are two of the best things for weight management and overall wellness. Learn more about these healthy habits.
From the latest fad diet to the newest supplement, nutrition information can be confusing and misleading. Here are some tips and resources from trusted health professionals to help you eat healthy and feel your best. Please talk with your health care provider or a registered dietitian if you have any health conditions.
Use MyPlate to plan healthy, well-balanced meals.
When you’re making a meal, try to include:
- ½ plate non-starchy veggies (like spinach, broccoli or peppers).
- ¼ plate lean protein (like low-fat cuts of red meat, chicken, seafood or tofu).
- ¼ plate whole grains, fruits or starchy vegetables (like potatoes, corn, peas or beans).
Reduce added sugar.
Some foods, like fruit, naturally have sugar. But there’s added sugar in many foods and drinks — like sodas, candies and desserts. A lot of other less-sweet foods also have added sugars, like salad dressings, condiments, pasta sauce, breads and cereals. When you’re choosing food, be sure to:
- Read the nutrition label to find out how much added sugar there is. It’s listed below the total sugar.
- Try to limit added sugar to no more than 36 grams per day (for men) or 24 grams per day (for women).
- Choose drinks without added sugar — like plain water, sparkling water, and unsweetened iced/hot tea or coffee.
- Avoid foods or drinks with high fructose corn syrup.
Avoid fad diets.
New diets come and go all the time. For instance, you may have heard of the keto or paleo diets — or other high-fat, high-protein and low-carb diets. For your health and safety, keep in mind that:
- Many diets claim to help with weight loss but can be very restrictive and hard to maintain long-term.
- Cutting out or greatly limiting certain groups of foods can lead to nutrient deficiencies. It is best to have different nutrients from all the food groups.
- Another popular way to diet, called intermittent fasting, may be helpful for weight loss, but it’s important that you talk with your health care provider or a registered dietitian first to make sure it’s appropriate for you. For example, it is not recommended if you have diabetes due to increased risk of hypoglycemia.
Try the Mediterranean approach if you’re looking for a diet.
If finding a diet is important to you, experts recommend the Mediterranean diet for overall health and a range of health conditions. It focuses on:
- Fruits and vegetables (at least 5 servings per day, such as 3 vegetables and 2 fruits).
- Lean proteins (like chicken, fish, eggs, beans and lentils), low-fat dairy products and healthy fats (like nuts, seeds, avocados and olive oil).
- More whole grains (like whole wheat bread or brown rice) and fewer refined grains (like white bread or white rice).
- More whole foods (like fruits, vegetables and nuts that are found in nature) and fewer processed foods (like chips, sodas or snack bars) overall.
WRITTEN BY
Lorraine Bonkowski, RDN, and Lauren Cornell, MS, RDN
Reviewed by DIGID Workgroup members ©June 2022
- Try moderate intensity activities like gardening, walking, biking, water aerobics and tennis. During moderate intensity exercise, you can still talk, but you can’t sing because you’re breathing faster than usual.
- Many people break up the 150 minutes a week into 30 minutes a day, 5 days a week. But do whatever works for your schedule and lifestyle. For instance, if it’s easier to fit in a couple of 10-minute walks each day rather than one longer one, that’s fine.
- If you can’t do 150 minutes each week, do what you can. Every little bit of movement helps, and you can always build up to more.
- Make your physical activity fun and convenient — that’s the best way to keep at it!
WRITTEN BY
Lorraine Bonkowski, RDN, and Lauren Cornell, MS, RDN
Reviewed by DIGID Workgroup members ©June 2022
Prescription drugs
Works by slowing down food leaving your stomach, which in turn slows down digestion.
Activates a part of the brain to regulate appetite and makes you feel full faster and for longer.
A mix of two medications, lowers appetite, helps with cravings and makes you feel full faster.
Works in the gut to reduce the amount of fat the body absorbs from food.
A mix of two medications, lowers appetite and makes you feel full faster.
Taken by injection for the treatment of genetic obesity caused by a rare single-gene mutation.
Other medications that help curb appetite include: benzphetamine, diethylpropion and phendimetrazine.
Endoscopic procedures
A device is attached to the outside of the body to reduce the number of calories absorbed.
Involves an injection directly into the stomach lining to freeze the stomach muscles, decreasing stomach contraction and slowing down digestion.
Surgical procedures
Your health care provider may discuss weight loss surgery with you if you have obesity and it poses risks to your health. These procedures involve sealing off a portion of the stomach (called restriction), and some also limit what your body can absorb (called malabsorption). They are significant surgeries that often involve weight loss beforehand. They usually require ongoing lifestyle changes and monitoring by your health care team.
Involves closing off 75% of the stomach with the remaining 25% forming a thin tube, or sleeve, that is joined to the intestines.
Often referred to as gastric bypass, it is a surgery that decreases the size of the stomach and causes food to bypass part of the small intestine, which limits calories and nutrients absorbed.
Reduces the size of the stomach opening and pouch, which makes you feel fuller faster.
Usually referred to as the duodenal switch, a complex surgery that reduces your ability to absorb calories, vitamins and minerals.
A complex surgery that reduces the size of the stomach and shifts digestive channel to limit the calories absorbed by the body.
Based on your health care provider’s recommendations, ask these important questions:
- How effective is this approach for most people?
- Would this be safe for me?
- What are the potential risks or side effects?
- What would I need to do before to get ready for the treatment?
- What will I need to do afterward to make sure this treatment is safe and effective?
Obesity, GERD and MASLD
Obesity can increase the risk of many health conditions, including gastroenterological conditions (also called GI conditions, which are related to the digestive system). Maintaining a healthy weight is a key factor in improving certain digestive health issues, including gastroesophageal reflux disease (GERD) and metabolic dysfunction-associated steatotic liver disease (MASLD).
Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the esophagus. While GERD is not life threatening, it can be very uncomfortable and impact your quality of life.
GERD is sometimes referred to as acid reflux. The most common symptom of GERD is frequent and severe heartburn.
Being overweight or having obesity is most likely causing your GERD symptoms or making your symptoms worse.
How can weight loss help with GERD?
Extra weight can put pressure on your abdomen, causing or worsening acid reflux. Losing weight can help remove extra fat and pressure around the abdomen, which can help you feel better.
What can I do next?
Here are some steps you can take today to address your GERD symptoms and find the weight loss option that’s right for you.
- View a video about obesity and health.
- Learn more about healthy eating and physical activity for GERD.
- Read about weight loss treatment options.
- Check out this decision tool before your next appointment with your gastroenterologist or other health care provider.
- Find out what weight loss options your insurance covers.
Metabolic dysfunction-associated steatotic liver disease (MASLD) occurs when your liver stores too much fat and it is not related to alcohol use. Nearly 40% of adults in the U.S. have MASLD, making it one of the most common liver diseases.
How can weight loss help with MASLD?
People who are overweight or have obesity are at a higher risk of MASLD. They are also more likely to have worse symptoms and eventually have metabolic dysfunction-associated steatohepatitis (MASH) or cirrhosis.
Weight loss can help reduce fat in the liver, inflammation (swelling) and fibrosis (scarring) associated with MASLD and MASH. If healthy weight is achieved in time, MASLD and MASH can be reversed.
What can I do next?
Here are some steps you can take today to address your MASLD symptoms and find the weight loss option that’s right for you:
- View a video about obesity and health.
- Learn more about healthy eating and physical activity for MASLD.
- Read about weight loss treatment options.
- Check out this decision tool before your next appointment with your gastroenterologist or other health care provider.
- Find out what weight loss options your insurance covers.
Insurance coverage
If you’re considering obesity or weight management counseling or treatment, you may want to know what your health insurance plan will — or will not — cover. Some weight loss programs, services and treatments are covered by insurance plans. But each plan is different, so it’s important to check with your insurance provider.
When you are discussing options with your health care provider, be sure to check your insurance coverage. Your health care provider may be able to recommend options that your insurance covers. For some options, you or your health care provider may need to ask for pre-approval from your insurance company.
Many health plans DO cover:
- Working with a dietitian or wellness coach on lifestyle changes, such as nutrition and physical activity.
- Certain prescription drugs and weight loss procedures.
Most health plans DO NOT cover:
- Surgical procedures for weight loss, especially if you haven’t tried other weight loss options first.
Don’t assume anything. Before starting a treatment, be sure to check with your insurance company to make sure it will be covered.
- Talk to your health care provider. Sometimes how a condition is diagnosed or described in your medical record impacts whether insurance will pay for treatment. Or your provider may be able to recommend a different option(s) that would be covered.
- Ask what the self-pay rate is for the treatment. Sometimes you can pay less if you are paying directly, without going through your insurance.
- Call your insurance company’s customer service department and ask:
- Why the treatment wouldn’t be covered.
- What evidence they would need to change the decision.
- What treatment options would be covered.
- If you have started treatment and then been denied coverage, you can appeal the decision. All insurance companies have a process to do this. Sometimes your health care provider can help you with the appeal process.
The American Gastroenterological Association (AGA) is a member of the Obesity Care Advocacy Network. As part of the network, AGA supports the Treat and Reduce Obesity Act (TROA).
TROA would expand Medicare to include prescription drugs for chronic weight management, behavioral counseling, and other prevention and treatment options.
Many private insurance companies base their coverage decisions on Medicare. So, if Medicare improves coverage for weight loss treatments, private insurance companies are likely to as well.
Reviewed by Andres Acosta, MD, PhD and Pooja Singhal, MD.
This program is supported by an independent grant from Novo Nordisk.
Questions and resources for every stage of your weight loss journey
Are you just starting out on your weight loss journey?
Do you want some help talking with your health care provider about weight loss?
Do you have GERD or MASLD and wonder if weight loss can help?
Do you want to know what weight loss options your health insurance covers?