What is Barrett’s esophagus?
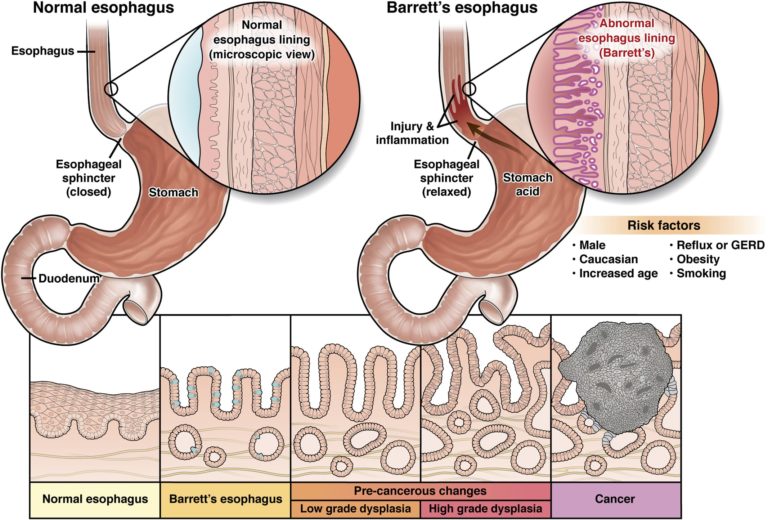
Having Barrett’s esophagus means the cells lining the esophagus (the tube that links the mouth and the stomach) have changed into types of intestinal cells that are not normal and increase the risk of long-term problems.
Barrett’s esophagus does not cause symptoms that you can feel. While the true cause is unknown, having heartburn that doesn’t go away could make you more likely to get Barrett’s esophagus.
It is found through an upper GI endoscopy and biopsy (taking a small piece of tissue to look at under a microscope). The biggest worry with Barrett’s esophagus is that those who have it are at a slightly greater risk for a type of cancer forming in the esophagus.
Once Barrett’s esophagus has been found, you should have an endoscopy done at regular intervals, suggested by your doctor, to look for pre-cancer cells (dysplasia).Who is at risk for Barrett’s esophagus?
Doctors do not know what exactly causes someone to get Barrett’s esophagus. There are a few things, though, that doctors have found could raise the chances of getting it. If you are worried that you could get Barrett’s esophagus, speak to your gastroenterologist.
- Men get Barrett’s esophagus twice as often as women.
- Caucasian men get it more often than men of other races.
- The average age at diagnosis is 55 years old.
- Between 5 and 15% of people with gastroesophageal reflux disease (GERD or reflux) get Barrett’s esophagus.
- Obesity — chiefly, high levels of belly fat — raises your chances of getting Barrett’s esophagus.
- Smoking raises your chances of getting Barrett’s esophagus.
- Some studies suggest that your genes may play a role in whether you get Barrett’s esophagus.
Tests for Barrett’s esophagus
The only way to find out if you have Barrett’s esophagus is with an endoscopy and a biopsy to look at the tissue of your esophagus (the tube that links your mouth and stomach) under a microscope.
Barrett’s esophagus can be hard to find, since it may not be in all the tissue in your esophagus. Because of this, the GI doing your endoscopy will take tissue samples (biopsies) from any areas of your esophagus that don’t look right.Endoscopy
An endoscopy is done to get small pieces of tissue (biopsies) from your esophagus (the tube that links your mouth and stomach) to see if the cells have changed. You will be given medicine to block pain and make you feel sleepy, so you won’t feel much during the test.
During the endoscopy, your gastroenterologist will use a long, thin (about the width of your little finger), flexible tube that has a tiny camera on the end.
After the test, a pathologist (a doctor who studies tissue) will look at the tissue in a lab to find out if Barrett’s esophagus cells are there.
Newly diagnosed with Barrett’s esophagus
Finding out if you have Barrett’s esophagus can seem like a lot, since the chance of future health concerns is higher. By talking openly with your health care provider, you can gain the facts needed to make choices that are right for you. Getting equipped with knowledge can help you feel more in control.
Things to keep in mind
- While you are at a higher risk for cancer than the general public, the individual risk of cancer or death is still relatively low (less than 1 in 200 patients with Barrett’s esophagus will get cancer each year).
- Before the cancer grows, your doctor can find pre-cancer cells and treat them.
- Once Barrett’s esophagus has been found, you should have an endoscopy done at regular intervals, suggested by your doctor, to look for pre-cancer cells (dysplasia).
Since there are no true symptoms of Barrett’s esophagus, you should take care of the symptoms that are bothering you from GERD or reflux, such as burning in your throat, a cough that won’t go away, loss of your voice and an upset stomach. Only when your doctor confirms Barrett’s esophagus should you think about specific treatments for it.
1. How often should I get an endoscopy?
2. Are there ways I can lower my risk of getting cancer?
3. Are there warnings that should cause worry?
Treatments for Barrett’s esophagus
Medication and daily habits
If you also have GERD along with Barrett’s esophagus, your doctor will have you start or stay on drugs to hold back the acid in your stomach. You can get these medications through your doctor, though you can also buy some without a prescription. Talk with your doctor about which choices are best for you before you take any medicines.
You can also help reduce reflux by staying away from certain foods like:
- Chocolate.
- Coffee.
- Peppermint.
- Greasy or fatty foods.
- Spicy foods.
- Alcohol.
Try eating small, well-balanced meals throughout the day.
Periodic surveillance endoscopy
In order to find any changes in the tissue in your esophagus (the tube that links your mouth and stomach) that could suggest pre-cancer cells or cancer, your gastroenterologist may choose endoscopic surveillance, or routinely taking a look at and removing some tissue. With this, your doctor is able to watch for signs of pre-cancer or cancer in the hopes of finding it early. Talk to your gastroenterologist about how often you need testing based on your disease.
Endoscopic eradication therapies
If you have cells that are highly abnormal in your tissue sample, or high-grade dysplasia, your doctor may suggest an endoscopic eradication therapy. These therapies not only kill the cells that are not normal, but they can also cause your body to start making normal esophageal cells.
These therapies are a bit more intense and are done at a hospital or an outpatient endoscopy center by a gastroenterologist.
- You will get medicine to numb your throat.
- You will get medicine to help you relax, so you should not feel pain during the procedure.
If you have any questions about these therapies, be sure to bring them up with your doctor.
Common forms of endoscopic eradication therapies
This therapy uses radio waves to kill pre-cancer and cancerous cells in the Barrett’s tissue. An electrode mounted on a balloon or an endoscope makes heat to kill the Barrett’s tissue and pre-cancer and cancerous cells.
Complications may include:
- Chest pain.
- Cuts in the lining of your esophagus.
- Strictures (narrowing of the esophagus).
Your doctor will lift the Barrett’s tissue, inject a solution underneath or apply suction to the tissue, and then cut the tissue off. The doctor then removes the tissue with an endoscope. Gastroenterologists do this procedure at certain hospitals and outpatient centers.
Doctors sometimes combine endoscopic mucosal resection with radiofrequency ablation or photodynamic therapy.
Complications may include:
- Bleeding.
- Tearing of your esophagus.
This therapy uses a light-activated chemical, an endoscope, and a laser to kill pre-cancer cells in your esophagus. A doctor injects the chemical into a vein in your arm, and you return 24 to 72 hours later to finish the procedure.
Complications may include:
- Sensitivity of your skin and eyes to light for about six weeks after the procedure.
- Burns, swelling, pain and scarring in nearby healthy tissue.
- Coughing, trouble swallowing, stomach pain, painful breathing and trouble breathing.
Surgery
Esophagectomy, surgery to remove some of the esophagus, may be an alternative to endoscopic eradication therapies if you have high-grade dysplasia (many abnormal or pre-cancer cells in the tissue).
Before proceeding to this option, you should be looked at by a surgical team that specializes in the care of Barrett’s esophagus with high-grade dysplasia. Surgery is often a last-resort treatment. Surgery may not be a choice if you have other health problems, because of the higher risks. Endoscopic eradication therapies are less invasive and often have fewer complications.